Other Nutrients
The Food and Nutrition Board of the US Institute of Medicine has set an Adequate Intake level for choline, essential fatty acids (linoleic acid and α-linolenic acid), and total fiber. Select a nutrient from the list for more information.
Choline
Contents
Summary
- Choline is a vitamin-like essential nutrient and a methyl donor involved in many physiological processes, including normal metabolism and transport of lipids, methylation reactions, and neurotransmitter synthesis. (More information)
- Choline deficiency causes abnormal deposition of fat in the liver, which results in a condition called nonalcoholic fatty liver disease. In some people, choline deficiency causes muscle damage. Genetic variants, sex, and hormonal status influence individual requirements and thus the susceptibility to choline deficiency-induced fatty liver disease. (More information)
- The recommended adequate intake (AI) of choline for Americans and Canadians is different across age groups and sex. For adults, the recommended intake is 425 milligrams (mg)/day for women and 550 mg/day for men. Dietary intake recommendations increase during pregnancy to 450 mg/day and during lactation to 550 mg/day. (More information) The vast majority of people living in the United States have dietary intakes below the AI. (More information)
- Choline is involved in the regulation of homocysteine concentration in the blood through its metabolite betaine. There is currently no convincing evidence that high choline intakes could benefit cardiovascular health by lowering blood homocysteine. (More information) Moreover, elevated blood concentrations of trimethylamine N-oxide (TMAO), generated from choline, have been associated with an increased risk of cardiovascular events in some observational studies. (More information)
- The need for choline is probably increased during pregnancy. Case-control studies examining the relationship between maternal choline status and risk of neural tube defects have given inconsistent results. It is not yet known whether periconceptional choline supplementation could confer protection against neural tube defects. (More information)
- Animal studies have shown that choline is essential for optimal brain development and influences cognitive function in later life. However, more human studies are needed to assert that choline supplementation during pregnancy improves cognitive performance in the offspring or that choline supplementation helps prevent cognitive decline in older people. (More information)
- While results of intervention studies are mixed, some evidence suggests that treatment with citicoline (a choline derivative) may be useful to improve retinal function in some patients with glaucoma. Citicoline has also been studied as a potential treatment to limit neurological damage in patients experiencing stroke or traumatic brain injury. (More information)
- De novo choline synthesis in humans is not sufficient to meet metabolic needs; therefore, choline intake from the diet is necessary. Good dietary sources of choline include eggs, meat, poultry, fish, cruciferous vegetables, peanuts, and dairy products. (More information)
-
Excessive consumption of choline (≥7,500 mg) has been associated with blood pressure lowering, sweating, fishy body odor, and gastrointestinal side effects. The tolerable upper intake level (UL) for adults is 3,500 mg/day. (More information)
Although choline is not by strict definition a vitamin, it is an essential nutrient. Despite the fact that humans can synthesize it in small amounts, choline must be consumed in the diet to maintain health. The majority of the body's choline is found in specialized fat molecules known as phospholipids, the most common of which is called phosphatidylcholine (1).
Function
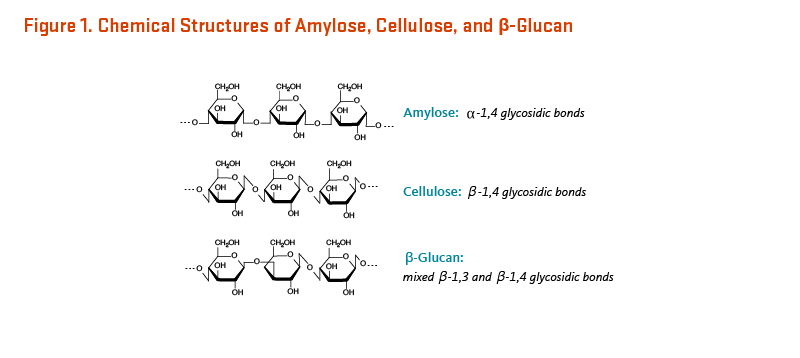
Choline and compounds derived from choline (i.e., metabolites) serve a number of vital biological functions (Figure 1) (1).
Structural integrity of cell membranes
Choline is used in the synthesis of certain phospholipids (phosphatidylcholine and sphingomyelin) that are essential structural components of cell membranes. Phosphatidylcholine accounts for about 95% of total choline in tissues (2). This phospholipid can be synthesized from dietary choline via the cytidine diphosphocholine (CDP-choline) pathway or through the methylation of another phospholipid, phosphatidylethanolamine (Figure 2) (3). Sphingomyelin is a type of sphingosine-containing phospholipid (sphingolipid) that is synthesized by the transfer of a phosphocholine residue from a phosphatidylcholine to a ceramide (Figure 3). Sphingomyelin is found in cell membranes and in the fatty sheath that envelops myelinated nerve fibers.
Cell signaling
The choline-containing phospholipids, phosphatidylcholine, and sphingomyelin, are precursors for the intracellular messenger molecules, diacylglycerol and ceramide. Specifically, sphingomyelinases (also known as sphingomyelin phosphodiesterases) catalyze the cleavage of sphingomyelin, generating phosphocholine and ceramide. Diacylglycerol is released by the degradation of phosphatidylcholine by phospholipases. Other choline metabolites known to be cell-signaling molecules include platelet-activating factor (PAF) and sphingophosphocholine.
Nerve impulse transmission
Choline is a precursor for acetylcholine, an important neurotransmitter synthesized by cholinergic neurons and involved in muscle control, circadian rhythm, memory, and many other neuronal functions. Choline acetyltransferase catalyzes the acetylation of choline to acetylcholine, and acetylcholine esterase hydrolyzes acetylcholine to choline and acetate (4). CDP-choline (citicoline) administration was also found to stimulate the synthesis and release of a family of neurotransmitters derived from tyrosine (i.e., the catecholamines, including noradrenaline, adrenaline, and dopamine) (5). Of note, non-neuronal cells of various tissues and organ systems also synthesize and release acetylcholine, which then binds and stimulates cholinergic receptors on target cells (reviewed in 6).
Lipid (fat) transport and metabolism
Fat and cholesterol consumed in the diet are transported to the liver by lipoproteins called chylomicrons. In the liver, fat and cholesterol are packaged into lipoproteins called very-low-density lipoproteins (VLDL) for transport in the bloodstream to extrahepatic tissues. Phosphatidylcholine synthesis by the phosphatidylethanolamine N-methyltransferase (PEMT) pathway is required for VLDL assembly and secretion from the liver (7, 8). Polymorphisms of the PEMT gene increase the dietary requirements of choline (9). Without adequate phosphatidylcholine, fat and cholesterol accumulate in the liver (see Deficiency).
Major source of methyl groups
Choline may be oxidized in the liver and kidney to form a metabolite called betaine via a two-step enzymatic reaction. In the mitochondrial inner membrane, flavin adenine dinucleotide (FAD)-dependent choline oxidase catalyzes the conversion of choline to betaine aldehyde, which is then converted to betaine by betaine aldehyde dehydrogenase in either the mitochondrial matrix or the cytosol (2). Betaine is a source of up to 60% of the methyl (CH3) groups required for the methylation of homocysteine (10). Betaine homocysteine methyltransferase (BHMT) uses betaine as a methyl donor to convert homocysteine to methionine in one-carbon metabolism (Figure 4). The ubiquitous vitamin B12-dependent methionine synthase (MS) enzyme also catalyzes the re-methylation of homocysteine, using the folate derivative, 5-methyltetrahydrofolate, as a methyl donor (see Nutrient interactions). Elevated concentrations of homocysteine in the blood have been associated with increased risk of cardiovascular disease (11).
Osmoregulation
The conversion of choline to betaine is irreversible. Betaine is an osmolyte that regulates cell volume and protect cell integrity against osmotic stress (especially in the kidney). Osmotic stress has been associated with a reduced BHMT expression such that the role of betaine in osmoregulation may be temporarily prioritized over its function as a methyl donor (2).
Deficiency
Symptoms
Men and women fed intravenously (IV) with solutions that contained adequate methionine and folate but lacked choline have been found to develop a condition called nonalcoholic fatty liver disease (NAFLD) and signs of liver damage that resolved when choline was provided (12). The occurrence of NAFLD is usually associated with the co-presentation of metabolic disorders, including obesity, dyslipidemia, insulin resistance, and hypertension, in subjects with metabolic syndrome. NAFLD is estimated to progress to a more severe condition called nonalcoholic steatohepatitis (NASH) in about one-third of NAFLD patients, as well as to increase the risk of cirrhosis and liver cancer (13).
Because phosphatidylcholine is required in the synthesis of very-low-density lipoprotein (VLDL) particles (see Function), choline deficiency results in impaired VLDL secretion and accumulation of fat in the liver (steatosis), ultimately leading to liver damage. Because low-density lipoprotein (LDL) particles are formed from VLDL particles, choline-deficient individuals also show reduced blood concentrations of LDL-cholesterol (14). Abnormally elevated biomarkers of organ dysfunction in the blood, including creatine phosphokinase, aspartate aminotransferase, and alanine aminotransferase, are corrected upon choline repletion. Choline deficiency-induced organ dysfunction has also been associated with increased DNA damage and apoptosis in circulating lymphocytes (15). In the liver, the accumulation of lipids is thought to impair mitochondrial function, thus reducing fatty acid oxidation and increasing the production of reactive oxygen species (ROS) that trigger lipid peroxidation, DNA damage, and apoptosis. Further, oxidative stress is thought to be responsible for prompting inflammatory processes that can lead to the progression of NAFLD to NASH and cirrhosis (end-stage liver disease) (16).
An intervention study in 57 healthy adults who were fed choline-deficient diets under controlled conditions found that 77% of men, 80% of postmenopausal women, and 44% of premenopausal women developed fatty liver, liver damage, and/or muscle damage (17). These signs of organ dysfunction resolved upon choline reintroduction in the diet. Because estrogen stimulates the endogenous synthesis of phosphatidylcholine via the phosphatidylethanolamine N-methyltransferase (PEMT) pathway, premenopausal women may be less likely to develop signs of choline deficiency in response to a low-choline diet compared to postmenopausal women (18, 19). Further, a notable single nucleotide polymorphism (SNP; rs12325817) of the PEMT gene, which may affect the expression and/or activity of the PEMT enzyme, is thought to increase the susceptibility to choline deficiency-induced organ dysfunction (18). Additional genetic polymorphisms occurring in choline and one-carbon metabolic pathways may alter the dietary requirement for choline and thus increase the likelihood of developing signs of deficiency when choline intake is inadequate (9, 20, 21).
Of note, the composition of one’s intestinal microbiota has been identified as a potential predictor of susceptibility to choline deficiency-induced NAFLD (22). Intestinal microbiota-dependent metabolism of dietary phosphatidylcholine might also be involved in the pathogenesis of cardiovascular disease (see Safety) (23, 24).
For more information on fatty liver diseases, see the section on Disease Prevention.
Individuals at risk of choline inadequacy
Daily intake recommendations are higher during pregnancy and lactation (see The AI), placing pregnant and lactating individuals at increased risk of choline inadequacy (25, 26). Vegetarians may also be at increased risk of choline inadequacy (26).
Patients with cystic fibrosis who have pancreatic insufficiency are at risk of choline depletion due to increased fecal losses (27). Circulating choline has been directly correlated with lung function in cystic fibrosis patients (28), and results of a pilot study in 10 patients suggested that choline supplementation may have utility in improving clinical outcomes in cystic fibrosis patients (29).
Nutrient interactions
Together with several B-vitamins (i.e., folate, vitamin B12, vitamin B6, and riboflavin), choline is required for the metabolism of nucleic acids and amino acids, and for the generation of the universal methyl group donor, S-adenosylmethionine (SAM) (Figure 4). SAM is synthesized from the essential amino acid, methionine. Three molecules of SAM are required for the methylation reaction that converts phosphatidylethanolamine into phosphatidylcholine (Figure 2). Once SAM donates a methyl group it becomes S-adenosylhomocysteine (SAH), which is then metabolized to homocysteine. Homocysteine can be converted back to methionine in a reaction catalyzed by vitamin B12-dependent methionine synthase, which requires 5-methyltetrahydrofolate (5-meTHF) as a methyl donor. Alternately, betaine (a metabolite of choline) is used as the methyl donor for the methylation of homocysteine to methionine by the enzyme, betaine-homocysteine methyltransferase (BHMT) (1). Homocysteine can also be metabolized to cysteine via the vitamin B6-dependent transsulfuration pathway (Figure 4).
Thus, the human requirement for choline is especially influenced by the relationship between choline and other methyl group donors, such as folate and S-adenosylmethionine. A low intake of folate leads to an increased demand for choline-derived metabolite, betaine. Moreover, the de novo synthesis of phosphatidylcholine is not sufficient to maintain adequate choline nutritional status when dietary intakes of folate and choline are low (30). Conversely, the demand for folate is increased when dietary supply for choline is limited (31).
The Adequate Intake (AI)
In 1998, the Food and Nutrition Board (FNB) of the Institute of Medicine (now the National Academy of Medicine) established a dietary reference intake (DRI) for choline (32). The FNB felt the existing scientific evidence was insufficient to calculate an RDA for choline, so they set an Adequate Intake (AI; Table 1). The main criterion for establishing the AI for choline was the prevention of liver damage. Yet, common polymorphisms in genes involved in choline or folate metabolism alter one’s susceptibility to choline deficiency and thus may affect dietary requirements for choline (see Deficiency) (18, 20, 33, 34).
Disease Prevention
Cardiovascular disease
Choline and homocysteine
A large body of research indicates that even moderately elevated levels of homocysteine in the blood increase the risk of cardiovascular disease (11). The most common cause of a myocardial infarction or a stroke is the rupture of atherosclerotic plaques in arterial walls causing blood clot formation (thrombogenesis). High homocysteine concentrations may promote the development of atherosclerosis (atherogenesis) and thrombogenesis via mechanisms involving oxidative stress and endothelial dysfunction, inflammation, abnormal blood coagulation, and disordered lipid metabolism (reviewed in 35).
Once formed from dietary methionine, homocysteine can be catabolized to cysteine via the transsulfuration pathway or re-methylated to methionine (Figure 4). Folate and choline are involved in alternate pathways that catalyze the re-methylation of homocysteine (see Nutrient interactions). Specifically, choline is the precursor of betaine, which provides a methyl group for the conversion of homocysteine to methionine via the enzyme, betaine-homocysteine methyltransferase (BHMT). While the amount of homocysteine in the blood is regulated by several nutrients, including folate and choline, conditions that cause damage to the liver like nonalcoholic steatohepatitis (NASH) may also affect homocysteine metabolism (36).
Dietary intakes of choline and betaine and risk of cardiovascular disease
Because both folate- and choline-dependent metabolic pathways catalyze the re-methylation of homocysteine, dietary intakes of both nutrients need to be considered when the association between homocysteine concentrations and cardiovascular disease is assessed. Yet, despite its relevance, the relationship of betaine and choline to homocysteine metabolism has been only lightly investigated in humans, essentially because the choline content of foods could not be accurately measured until fairly recently. In preliminary intervention studies, pharmacologic doses of betaine (1,500 to 6,000 mg/day) were found to reduce blood homocysteine concentrations in a small number of volunteers with normal-to-mildly elevated homocysteine concentrations (37-40). Yet, in a cross-sectional analysis of a large cohort of 16,165 women (ages, 49-79 years), lower betaine doses in the range of dietary intakes were not found to be correlated with homocysteine concentrations (41). This study also showed that levels of choline intake were inversely associated with homocysteine concentrations in the blood. However, an eight-year follow-up study of the cohort failed to show any difference in cardiovascular risk between women in the upper versus bottom quartile of dietary choline intakes (>329 mg/day vs. ≤266 mg/day) (41).
More recent prospective cohort studies on the association of dietary choline or betaine and cardiovascular disease have been mixed. In the Jackson Heart Study, which followed 3,924 African Americans for nine years, higher dietary choline intakes were associated with a reduced risk of stroke (42). In the Nurses’ Health Study (80,978 women) and the Health Professionals Follow-up Study (39,434 men), higher dietary intakes of phosphatidylcholine were linked to a higher risk of cardiovascular disease-related mortality (43). Higher total daily choline intakes were linked to a higher risk of cardiometabolic mortality (i.e., death attributed to cardiovascular disease or type 2 diabetes mellitus) in large prospective cohorts of three ethnic groups: blacks (n=49,858), whites (n=23,766), and Chinese (n=134,001) (44). In this study, higher betaine intakes were associated with a higher risk of cardiometabolic death in the Chinese cohort only (44). However, no associations between choline or betaine intakes and cardiovascular-related mortality were found in a cohort study of Japanese adults (n=29,079) (45). Several other prospective cohort studies have failed to find an association between choline intake and cardiovascular disease endpoints (41, 46-48).
Convincing evidence that increased dietary intake of choline or betaine could benefit cardiovascular health through lowering homocysteine concentrations in the blood is presently lacking.
Circulating concentrations of choline and betaine and risk of cardiovascular disease
A 1995 study had found that elevated blood homocysteine concentrations in patients who experienced a vascular occlusion were associated with higher urinary excretion of betaine, rather than with reduced intake of choline or betaine or diminished activity of BHMT (49). In a prospective study, high urinary betaine excretion was also associated with increased risk of heart failure in 325 subjects without diabetes mellitus who had been hospitalized for acute coronary syndrome (50). In the same study, both top and bottom quintiles of plasma betaine concentrations were associated with an increased risk of secondary acute myocardial infarction. The findings of another prospective study (the Hordaland Health Study) that followed 7,045 healthy adults (ages, 47-49 years and 71-74 years) suggested that high choline and low betaine plasma concentrations were associated with an unfavorable cardiovascular risk profile (51). Indeed, plasma choline was positively associated with a number of cardiovascular risk factors, such as BMI, percentage body fat, waist circumference, and serum triglycerides, and inversely associated with HDL-cholesterol. On the contrary, plasma betaine was positively correlated to HDL-cholesterol and inversely associated with the above-mentioned risk factors, as well as with systolic and diastolic blood pressure.
More recent studies suggest that the blood concentration of trimethylamine N-oxide (TMAO), generated from trimethylamine-containing nutrients like dietary choline, rather than that of choline, might influence the risk of cardiovascular events (see Safety). However, the association between high blood levels of TMAO and atherosclerosis was not observed in the Coronary Artery Risk Development in Young Adults Study (CARDIA) (52)
It is not yet clear whether concentrations of choline, betaine, and/or TMAO in the blood can predict the risk for cardiovascular disease.
Liver diseases
Fatty liver diseases
While a choline-deficient diet results in organ dysfunction and nonalcoholic fatty liver disease (NAFLD) (see Deficiency; 17), it is not known whether suboptimal dietary choline intakes in healthy subjects may contribute to an increased risk for NAFLD. A cross-sectional analysis of two large prospective studies conducted in China — the Shanghai Women’s Health Study and the Shanghai Men’s Health Study — including 56,195 people (ages, 40-75 years), was conducted to assess the association between dietary choline intakes and self-reported diagnosis of fatty liver disease (53). The highest versus lowest quintile of choline intake (412 mg/day vs. 179 mg/day) was associated with a 28% lower risk of fatty liver disease in normal-weight women, but no association was found in overweight or obese women or in men. Another cross-sectional study of 664 individuals with NAFLD or nonalcoholic steatohepatitis (NASH) also reported that disease severity was inversely correlated with dietary choline intakes in postmenopausal women, but not in premenopausal women, men, or children (54). Moreover, in a US national cross-sectional survey of 20,643 adults, higher dietary intakes of choline were associated with a more favorable profile of liver enzymes and with a lower risk of developing NAFLD (NHANES 2005-2012) (55).
Liver cancer
In animal models, dietary choline deficiency has been associated with an increased incidence of spontaneous liver cancer (hepatocellular carcinoma) and increased sensitivity to carcinogenic chemicals (10). A number of mechanisms have been proposed to contribute to the cancer-promoting effects of choline deficiency: (1) enhanced liver cell regeneration and tissue sensitivity to chemical insults; (2) altered expression of numerous genes regulating cell proliferation, differentiation, DNA repair, and apoptosis due to improper DNA methylation; (3) increased likelihood of DNA damage caused by mitochondrial dysfunction-induced oxidative stress; and (4) activated protein kinase C-mediated cell-signaling cascade, eventually leading to an increase in liver cell apoptosis (2). Yet, it is not known whether choline deficiency can increase the susceptibility to cancer in humans (2).
Neural tube defects
It is known that folate is critical for normal embryonic development, and maternal supplementation with folic acid decreases the incidence of neural tube defects (NTDs) (56). NTDs include various malformations, such as lesions of the brain (e.g., anencephaly, encephalocele) or lesions of the spine (spina bifida), which are devastating and usually incompatible with life (57). These defects occur between the 21st and 28th days after conception, a time when many women do not realize that they are pregnant (58). While the protective effect of folate against NTD is well established, only a few studies have investigated the role of other methyl group donors, including choline and betaine, in the occurrence of NTDs. A case-control study (424 NTD cases and 440 controls) found that women in the highest versus lowest quartile of periconceptual choline intake (>498.46 mg/day vs. ≤290.41 mg/day) had a 51% lower risk of an NTD-affected pregnancy (59). However, more recent studies have failed to find an inverse relationship between maternal choline intake and risk of NTDs (60-63).
A case-control study (80 NTD-affected pregnancy and 409 controls) in US women found that the lowest concentrations of serum choline (<2.49 mmol/L) during mid-pregnancy were associated with a 2.4-fold higher risk of NTDs (64). Finally, a more recent study, including 71 NTD-affected pregnancies, 214 pregnancies with non NTD malformations, 98 normal pregnancies in women with prior NTD-affected pregnancies, and 386 normal pregnancies, found no associations between maternal blood concentrations of choline during pregnancy, choline- and folate-related genetic variants, and risk of NTDs (65). However, it is important to note that circulating choline concentrations do not accurately reflect dietary intake of choline.
In a recent meta-analysis that pooled the results of five case-control studies (59, 60, 62-64), including 1,131 NTD-affected pregnancies and 4,439 healthy controls, lower dietary choline intakes or lower serum concentrations of choline were associated with a 36% higher risk of NTDs compared to higher levels (95% CI, 1.11, 1.67) (66).
Randomized controlled trials of choline supplementation throughout the periconceptional period would been needed to determine whether choline has a protective effect against NTDs.
Cognitive health
Neuro-cognitive development
Increased dietary intake of cytidine 5’-diphosphocholine (CDP-choline or citicoline, a precursor of phosphatidylcholine; Figure 2) very early in life can diminish the severity of memory deficits in aged rats (67). Choline supplementation of the mothers of unborn rats, as well as rat pups during the first month of life, led to improved performance in spatial memory tests months after choline supplementation had been discontinued (68). A review by McCann et al. discusses the experimental evidence from rodent studies regarding the availability of choline during prenatal development and cognitive function in the offspring (69).
Because of the importance of DNA methylation in normal brain development, neuronal functions, and cognitive processes (70), methyl donor nutrients like choline are essential for optimal brain functioning. However, clinical evidence to determine whether findings in rodent studies are applicable to humans is currently limited. The analysis of the Seychelles Child Development Nutrition Cohort study reported a lack of an association between plasma concentrations of choline and its related metabolites and cognitive abilities in 256 five-year-old children. Only plasma betaine concentrations were found to be positively correlated with preschool language test scores (71). Yet, because circulating concentrations of choline are not directly related to dietary choline intakes, the study could not evaluate whether maternal choline intakes influence children’s brain development.
Project Viva is an ongoing prospective study that has examined the relationship between daily intakes of methyl donor nutrients in 1,210 women during pregnancy and child cognition at three and seven years postpartum. Maternal intake of choline during the first and/or second trimester of pregnancy was not correlated with measures of cognitive performance in children at age 3 years (72). Another report of the study indicated that upper versus lower quartile of maternal choline intakes during the second trimester of pregnancy (median intakes, 392 mg/day vs. 260 mg/day) was significantly associated with higher visual memory scores in children ages 7 years old (73). In addition, a small randomized, double-blind, placebo-controlled trial in 99 pregnant women (ages, 21-41 years old) evaluated the effect of choline supplementation during pregnancy and lactation on infants’ cognitive function at ages 10 and 12 months (74). The results indicated that maternal choline supplementation (750 mg/day of choline in the form of phosphatidylcholine) from 18 weeks of gestation to 3 months’ postpartum provided no cognitive benefits in children regarding short-term visuospatial memory, long-term episodic memory, and language and global development (74). In a randomized, double-blind, controlled-feeding study in 24 pregnant women, maternal choline intake of 930 mg/day (~2x the AI) throughout the third trimester of pregnancy improved measures of information-processing speed (i.e., reaction times) and visuospatial memory in infants compared to choline intakes of 480 mg/day (75). Choline intake in this study was from both dietary and supplemental sources: 380 mg/day of choline from dietary sources and either 100 mg/day or 550 mg/day from supplemental choline chloride (75). Follow-up of the offspring (N=20) at 7 years of age indicated that children of mothers who consumed 930 mg/day of choline had higher measures of sustained attention compared to those of mothers who consumed 480 mg/day of choline (76), suggesting that prenatal choline supplementation during late pregnancy can confer cognitive benefits to the child.
Cognitive function in older adults
Cognitive function, including the domains of memory, speed, and executive function, decline gradually with increasing age. The rate of cognitive decline is also influenced by modifiable risk factors like dietary habits. Deficiency in B-vitamins and elevated blood concentrations of homocysteine have been associated with cognitive impairments in the elderly. A recent meta-analysis of 14 randomized, placebo-controlled trials found that B-vitamin supplementation slowed cognitive decline in cognitive healthy older adults, as measured by score on the Mini-Mental State Examination, compared to placebo (77). However, less is known about dietary or supplemental choline specifically.
A few observational studies have examined choline intake and cognitive function in older adults, but these are cross-sectional in nature. The cross-sectional data analysis of a subgroup of 1,391 volunteers (ages, 36-83 years) from the large Framingham Heart Study Offspring cohort has indicated that dietary choline intake was positively associated with specific cognitive functions, namely verbal memory and visual memory (78). In a US national cross-sectional study of 2,393 older adults (≥60 years), total daily choline intakes (combined from diet and supplements) between 187.06 and 399.5 mg/day were associated with improved cognitive performance in three separate measures (assessing learning, processing speed, sustained attention, and working memory) compared to intakes less than 187.06 mg/day; however, the highest intakes of choline (>399.5 mg/day) were no different than the lowest intakes (<187.06 mg/day) in these measures (79).
Another cross-sectional study of 2,195 older individuals (ages, 70-74 years) from the Hordaland Health Study examined cognitive abilities and blood concentrations of various determinants of circulating homocysteine, including choline and betaine (80). Unlike betaine, high versus low plasma concentrations of free choline (>8.36 µM vs. ≤8.36 µM) were found to be significantly associated with a greater performance at cognitive tests assessing sensory motor speed, perceptual speed, executive function, and global cognition. However, in an earlier intervention study that enrolled 235 elderly individuals (mean age, 81 years old) with or without mild vitamin B12 deficiency, baseline concentrations of betaine — but not choline — were found to be positively correlated to test scores evaluating the cognitive domains of construction, sensory motor speed, and executive function (81).
More research is needed to determine the effect of choline on the developing brain and whether choline intakes above the RDA may be useful in the prevention of memory loss or dementia in older adults.
Disease Treatment
Neurodegenerative diseases
Dementia
Neurodegenerative diseases, such as Alzheimer's disease (AD) and Parkinson’s disease (PD), are characterized by progressive cognitive decline and dementia. Dysfunctions in neurotransmitter signaling, affecting cholinergic and dopaminergic pathways in particular, have been involved in the occurrence of cognitive impairments. Deficits in acetylcholine and abnormal phospholipid metabolism have been reported in postmortem studies of the brains of AD patients (12). For these reasons, inhibitors of (acetyl) cholinesterase (which catalyzes the breakdown of acetylcholine) and large doses of lecithin (phosphatidylcholine) have been used to treat patients with dementia due to AD in hopes of raising the amount of acetylcholine available in the brain. While cholinesterase inhibitors have shown positive effects on cognitive functions and measures of clinical global state (82), a systematic review of randomized controlled trials did not find lecithin to be more beneficial than placebo in the treatment of patients with cognitive impairment, vascular dementia, AD, or mixed dementia (83). Limited data — mostly from case-control studies — are available to assess whether citicoline (CDP-choline) might improve cognitive performance in subjects with AD or PD, and studies to date have generally been labeled as poor in quality (84).
Glaucoma
Optic neuropathies, including glaucoma, are associated with damage of the optic nerve and loss of visual function. In glaucoma, the progressive deterioration of the optic nerve is caused by loss of a specific neuronal population known as retinal ganglion cells (RGC), such that the condition has been classified as a neurodegenerative disease (85). Choline and its metabolites have a number of roles in supporting normal visual function, including retinal function (86).
In a small, double-blind, placebo-controlled study, the effect of citicoline was assessed in 24 subjects affected by open-angle glaucoma and treated with β-blockers. Patients were randomized to follow a therapeutic cycle for a total period of eight years: citicoline (1,000 mg/day, by intramuscular injection) or placebo (β-blockers alone) for a two-month period followed by a four-month washout period (87). Electrophysiological examinations were used to assess the extent of visual dysfunctions, including the simultaneous recordings of Pattern ElectroRetinoGrams (PERG) and Visual Evoked Potentials (VEP). Citicoline was found to enhance retinal function and neural conduction along post-retinal visual pathways, such that responses of the visual cortex to stimuli were significantly improved compared to placebo (87).
In a similar pilot trial, citicoline efficacy was assessed in 26 volunteers (mean age, 65.4 years) affected by another type of optic neuropathy known as non-arteritic anterior ischemic optic neuropathy (NAION). Oral citicoline (1,600 mg/day) was given for 60 days followed by 60 days of washout, and the therapeutic cycle was repeated once. Compared to placebo, citicoline was found to improve retinal function and post-retinal neural conduction, evidenced by PERG and VEP measures (88). Oral citicoline (four cycles of 500 mg/day for four months followed by a two-month washout period) was also found to significantly reduce the rate of visual field loss and the level of intraocular pressure in 41 patients with progressive glaucoma (89). Larger randomized controlled trials are needed to establish whether citicoline supplementation could be included in the medical treatment of glaucoma.
A few studies have also explored topical citicoline (i.e., eyedrops) as a potential treatment for glaucoma. One study in 56 patients with open-angle glaucoma found that such topically applied citicoline for four months improved retinal function and visual-related neural conduction when on top of β-blocker monotherapy to lower intraocular pressure (90). In a randomized, double-blind, placebo-controlled trial in 78 patients with progressive open-angle glaucoma (despite intraocular pressures of ≤18 mm Hg), use of citicoline eyedrops for three years blunted the decrease in retinal nerve fiber layer thickness compared to use of placebo eyedrops (91). This trial also found a trend (p=0.07) for a lower rate of disease progression with topical citicoline (91). While the results of these pilot studies are promising, large-scale randomized controlled trials are needed.
Cerebrovascular diseases
Cerebrovascular diseases (including stroke and sub-acute ischemic cerebrovascular disease) are the main cause of cognitive impairments in older people. Results from experimental studies have suggested that pharmacological doses of citicoline (CDP-choline) could enhance the metabolism of glucose and the biosynthesis of phospholipids and neurotransmitters, while limiting the degradation of phospholipids in neuronal membranes in models of ischemia and neurodegenerative diseases (reviewed in 92). Many short-term intervention studies in older individuals with vascular diseases have found that therapeutic doses of citicoline — given orally, by intramuscular injection, or by intravenous infusion — resulted in improvements in neuropsychological functions, including cognitive, emotional, and behavioral functions (reviewed in 5).
A six-month, multicenter observational study enrolled 197 stroke subjects (mean age, 81.5 years) with a progressive decline of their mental health and general confusion and/or stupor who were initially administered citicoline for 5 or 10 days (2,000 mg/day, by intravenous infusion) within a four-month period, and then for 21 days (1,000 mg/day, by intramuscular injection), repeated once after a seven-day washout period (93). Citicoline treatment was found to be associated with higher scores on cognitive and functional evaluation scales when compared to baseline measurements. However, only randomized controlled trials would be able to assess whether citicoline is protective against vascular damage and cognitive impairment in elderly adults with complex geriatric symptoms.
The International Citicoline Trial on acUte Stroke (ICTUS) is a multicenter and double-blind study that assessed the effect of supplementing 2,298 patients with acute ischemic stroke with citicoline (2,000 mg/day) or a placebo for six weeks on several functional and neurologic outcomes and on mortality rate (94). The results showed no difference between treatment groups after a 90-day follow-up period. Only subgroup analyses found significant benefits of citicoline in patients older than 70 years, in those with moderate rather than severe strokes, and in those not treated with recombinant tissue plasminogen activator (rtPA; standard-of-care treatment). An earlier meta-analysis of small randomized, placebo-controlled trials had reported a positive impact of citicoline (1,000 mg/day, administered for 28 days to 12 months) on memory and behavior in subjects with cognitive deficits associated with cerebrovascular disorders (95). The effect of citicoline was also evaluated in a multicenter, open-label, controlled trial (IDEALE trial) in Italian elderly adults (ages, 65-94 years) with evidence of vascular lesions on neuroradiology and mild-to-moderate cognitive deficits, as assessed by Mini-Mental State Examination (MMSE; scores ≥21) (96). Three hundred and forty-nine participants received oral citicoline (1,000 mg/day) or no treatment for nine months. MMSE scores in citicoline-treated individuals remained unchanged while they significantly deteriorated in untreated patients such that MMSE scores between groups were found to be significantly different after three and nine months of treatment. No significant effect was reported in measures of functional autonomy, mood, and behavioral disorders. Another open-label, randomized, controlled trial evaluated the effect of citicoline (1,000 mg/day for 12 months) in 347 subjects (mean age, 67.2 years) who suffered an acute stroke. The results demonstrated that citicoline significantly limited cognitive impairments in the domains of attention and executive functions and temporal orientation at 6 and 12 months post-stroke in treated compared to untreated patients (97). However, other randomized controlled trials have not found any benefit of citicoline treatment in the management of acute ischemic stroke (98, 99), including a recent trial evaluating its effects when provided immediately following endovascular thrombectomy (i.e., recanalization therapy) and continued for 42 days (100). A systematic review and meta-analysis of 10 randomized controlled trials found that citicoline therapy in acute ischemic stroke (provided intravenously and/or orally between 8 hours and 14 days post stroke) was linked to a slightly higher rate of independence (101). However, a recent Cochrane review of randomized controlled trials found that citicoline had no benefit to acute ischemic stroke patients compared to placebo with respect to all-cause mortality (8 trials); serious, adverse cardiovascular events (3 trials); or degree of disability or dependence with daily tasks (4 trials) (102).
Thus, there is little evidence that citicoline treatment is efficacious for patients with cerebrovascular disease. Many of the conducted trials have not been a double-blind design, which reduces the risk of bias.
Traumatic brain injury
For decades, preclinical and small clinical studies have investigated the effect of citicoline — when provided intravenously, intramuscularly, or orally — in the management of traumatic brain injury (TBI). A 2011 systematic review of clinical data suggested that citicoline could hasten the resorption of cerebral edema and improve the recovery of consciousness and neurologic disorders in severe TBI cases (classified by Glasgow Coma Scale [GCS] scores of ≤8) (5). Citicoline also appeared to limit memory deficits and the duration and severity of other post-traumatic symptoms (e.g., headache, dizziness, attention disorder) in TBI patients with mild-to-moderate injuries (GCS scores, 9-15) (reviewed in 5).
Although citicoline is included in TBI therapeutic regimen in 59 countries, only one multicenter, randomized, double-blind, placebo-controlled trial has been conducted in the US. The CiticOline Brain Injury Trial (COBRIT) has enrolled 1,213 patients with mild-to-severe TBI and assessed the effect of enteral or oral citicoline (2,000 mg/day, for 90 days) on functional and cognitive outcomes (measured by components of the TBI Clinical Trials Network Care Battery) (103). No significant benefits of citicoline supplementation over placebo were found at 90 days (end of treatment period) and 180 days. It is important to note that this trial had low adherence: only 44% of patients in the trial took at least 75% of their assigned dose (103). When pooling the results of COBRIT with those of 10 other clinical trials in a meta-analysis, citicoline treatment for acute-phase TBI was linked to a higher degree of independence, i.e., the capability of performing daily activities without needing assistance (104).
Sources
De novo synthesis (biosynthesis)
Humans can synthesize choline moieties in small amounts by converting phosphatidylethanolamine into phosphatidylcholine (Figure 2). Three methylation reactions catalyzed by phosphatidylethanolamine N-methyltransferase (PEMT) are required, each using S-adenosylmethionine (SAM) as a methyl group donor. Choline is generated endogenously when the methylation of phosphatidylethanolamine is coupled with the catabolism of newly formed phosphatidylcholine by phospholipases. This is referred to as de novo synthesis of choline. The substitution of choline by serine in the synthesis of phosphatidylserine from phosphatidylcholine by phosphatidylserine synthase-1 also releases choline (4). Because phosphatidylcholine metabolism is a source of endogenous choline, the nutrient was not initially classified as essential (1). Yet, de novo choline synthesis in humans is not sufficient to meet their metabolic needs such that healthy humans fed choline-deficient diets develop fatty liver, liver damage, and/or muscle damage (see Deficiency).
Food sources
In the US, mean dietary intakes of choline are well below the recommended Adequate Intake (AI) level. According to a US national survey, NHANES 2015-2018, mean dietary intakes of choline were 284 mg/day for women and 390 mg/day for men; only 6% of women and 11% of men had dietary intakes greater than the AI (105). Moreover, NHANES data indicate that less than 9% of pregnant women meet the AI for choline (106). Americans of all ages have low intakes of choline: an analysis of NHANES 2009-2012 found that less than 11% of US residents ages 2 years and older had total choline intakes (from diet and supplements combined) above the AI (107). Stratifying the data by life stage indicated that young children ages 2-8 years were more likely to meet the AI than older children, adolescents, or adults (107). Vegetarians, especially vegans, who consume no meat, milk, or eggs, may be at risk for inadequate choline intake (26).
Eggs, liver, cruciferous vegetables, and peanuts are especially rich in choline (32, 108); one analysis of NHANES data concluded that it is extremely difficult to meet the AI from food sources alone if eggs are not consumed (106). Major contributors to choline in the American diet are meat, poultry, fish, dairy foods, pasta, rice, and egg-based dishes (109). Spinach, beets, wheat, and shellfish are also good sources of the choline metabolite, betaine (110). Betaine cannot be converted back to choline but can spare some choline requirements for homocysteine remethylation (1).
Phosphatidylcholine, which contains about 13% choline by weight, is the main form of choline in dietary products (111). Lecithin extracts, which comprise a mixture of phosphatidylcholine and other phospholipids, are often added during food processing. Lecithins in processed food have been estimated to increase the daily consumption of phosphatidylcholine by about 1.5 mg/kg of body weight for adults (32).
The total choline contents of some choline-containing foods are listed in milligrams (mg) in Table 2. For more information on the nutrient content of specific foods, search USDA’s FoodData Central or the USDA’s documentation on the choline content of common foods.
Supplements
CDP-choline (citicoline) and choline salts, such as choline chloride and choline bitartrate, are available as supplements. Phosphatidylcholine supplements also provide choline; however, choline comprises only about 13% of the weight of phosphatidylcholine (111). Therefore, a supplement containing 4,230 mg (4.23 grams) of phosphatidylcholine would provide 550 mg of choline. Although the term "lecithin" is synonymous with phosphatidylcholine when used in chemistry, commercial lecithins are usually prepared from soybean, sunflower, and rapeseed, and may contain anywhere from 20%-90% of phosphatidylcholine. Egg yolk lecithin is a more unlikely source of lecithin in dietary supplements. Moreover, the nature of phosphatidylcholine-containing fatty acids depends on whether lecithin is produced from vegetable, animal, or microbial sources. In particular, soybean lecithin is richer in polyunsaturated fatty acids than egg yolk lecithin (112).
Most multivitamin supplements, including prenatal multivitamins, do not contain choline; the few that do often contain choline at levels much lower than the AI (113).
Safety
Toxicity
High doses (10,000 to 16,000 mg/day) of choline have been associated with a fishy body odor, vomiting, salivation, and increased sweating. The fishy body odor results from excessive production and excretion of trimethylamine, a metabolite of choline. In the inherited condition, primary trimethylaminuria (also known as "fish odor syndrome"; see the article on Riboflavin), a defective flavin containing monooxygenase 3 (FMO3) enzyme results in impaired oxidation of trimethylamine in the liver. Disease management includes the use of choline-restricted diets in affected individuals (114). Taking large doses of choline in the form of phosphatidylcholine (lecithin) does not generally result in fishy body odor, because its metabolism results in little trimethylamine.
A dose of 7,500 mg/day of choline was found to have a slight blood pressure-lowering (hypotensive) effect, which could result in dizziness or fainting. Choline magnesium trisalicylate at doses of 3,000 mg/day has resulted in impaired liver function, generalized itching, and ringing of the ears (tinnitus). However, it is likely that these effects were caused by the salicylate, rather than the choline in the preparation (32).
In 1998, the Food and Nutrition Board (FNB) of the Institute of Medicine (now the National Academy of Medicine) established the tolerable upper intake level (UL) for choline at 3,500 mg/day for adults (Table 3). This recommendation was based primarily on preventing hypotension (low blood pressure), and secondarily, on preventing the fishy body odor due to increased excretion of trimethylamine. The UL was established for generally healthy people, and the FNB noted that individuals with liver or kidney disease, Parkinson's disease, depression, or inherited trimethylaminuria might be at increased risk of adverse effects when consuming choline at levels near the UL (32).
Do high choline intakes and/or phosphatidylcholine supplements increase the risk for cardiovascular disease?
Oral supplementation with phosphatidylcholine (250 mg of total choline from food plus 250 mg of supplemental phosphatidylcholine) has been found to result in detectable concentrations of trimethylamine and trimethylamine N-oxide (TMAO) in the blood (23). The intestinal microbiota is directly implicated in the generation of trimethylamine from dietary choline and its metabolite phosphatidylcholine, as well as from dietary betaine and carnitine. Trimethylamine is subsequently converted into TMAO by flavin-containing monooxygenases in the liver. The prospective study that followed 4,007 individuals — with or without cardiovascular disease — for a three-year period found baseline concentrations of circulating TMAO to be positively correlated with incidence of death, nonfatal myocardial infarction, and stroke — described as major adverse cardiac events (MACE) (23). In the same cohort, MACE risk was found to be about 30% higher in individuals in the highest versus lowest quartile of choline or betaine plasma concentrations (115). However, depending on gut microbiota composition, the risk of having an adverse cardiovascular event may be lower in individuals with low versus high circulating TMAO even though choline and/or betaine concentrations in the blood are elevated (115). Similar findings have since been made in other prospective cohorts. A meta-analysis of 19 prospective studies found that higher blood TMAO concentrations were associated with a 62% increased risk for MACE or death compared to lower concentrations (116). Elevated circulating TMAO concentrations have been not only linked to an increased risk of cardiovascular disease but also to an increased risk for type 2 diabetes mellitus and kidney disease (117-119). However, high TMAO concentrations in blood may be a biomarker of the disease rather than a causative factor (120, 121).
Further research is needed to understand how the composition of intestinal microbiota influences the metabolic fate of ingested choline. At present, there is little evidence that dietary choline increases the risk of cardiovascular events. Prospective cohort studies on the association have been inconsistent: a few studies have linked higher choline intakes to increased risks of atrial fibrillation (122) and cardiovascular disease-related mortality (43, 44), while several other prospective studies have found no association between choline intake and cardiovascular disease endpoints (41, 45-48). Interestingly, in the PREvención con DIeta MEDiterránea-Plus (Predimed-Plus) trial in overweight or obese individuals with metabolic syndrome, an increase in dietary choline intake over a one-year period was associated with improved measures of cardiovascular health (i.e., lower serum total cholesterol, serum LDL cholesterol, and systolic and diastolic blood pressure levels) (123).
Drug interactions
Methotrexate, a medication used in the treatment of cancer, psoriasis, and rheumatoid arthritis, inhibits the enzyme dihydrofolate reductase and therefore limits the availability of methyl groups donated from folate derivatives. Rats given methotrexate have shown evidence of diminished nutritional status of choline and greater drug adverse reactions due to liver dysfunction (12, 124). Thus, individuals taking methotrexate may have an increased choline requirement. Treatments with a family of lipid-lowering drugs known as fibrates (e.g., fenofibrate, bezofibrate) have been associated with an increased excretion of betaine in the urine and a rise in homocysteine concentration in the blood of patients with diabetes mellitus or metabolic syndrome (125, 126). If the benefits of fibrate therapy are indeed mitigated by fibrate-induced betaine deficiency, the use and safety of supplementing patients with betaine would need to be considered (127).
Linus Pauling Institute Recommendation
Little is known regarding the amount of dietary choline required to promote optimum health or prevent chronic diseases in humans. The Linus Pauling Institute supports the recommendation by the Food and Nutrition Board of 425 mg/day for adult women and 550 mg/day for adult men. A varied, healthy diet should provide enough choline for most people, but strict vegetarians who consume no milk or eggs may be at risk of inadequate choline intake.
Older adults (>50 years)
Little is known regarding the amount of dietary choline most likely to promote optimum health or prevent chronic diseases in older adults. At present, there is no evidence to support a different recommended intake of choline from that of younger adults (425 mg/day for women and 550 mg/day for men).
Authors and Reviewers
Originally written in 2000 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in May 2003 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in January 2008 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in August 2009 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in January 2015 by:
Barbara Delage, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in April 2023 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Reviewed in July 2023 by:
Isis Trujillo-Gonzalez, Ph.D.
Assistant Professor
Nutrition Research Institute
University of North Carolina at Chapel Hill
Copyright 2000-2025 Linus Pauling Institute
References
1. Zeisel SH, Corbin KD. Choline. Present Knowledge in Nutrition. 10th ed: John Wiley & Sons, Inc.; 2012:405-418.
2. Ueland PM. Choline and betaine in health and disease. J Inherit Metab Dis. 2011;34(1):3-15. (PubMed)
3. Gibellini F, Smith TK. The Kennedy pathway--De novo synthesis of phosphatidylethanolamine and phosphatidylcholine. IUBMB Life. 2010;62(6):414-428. (PubMed)
4. Li Z, Vance DE. Phosphatidylcholine and choline homeostasis. J Lipid Res. 2008;49(6):1187-1194. (PubMed)
5. Secades JJ. Citicoline: pharmacological and clinical review, 2010 update. Rev Neurol. 2011;52 Suppl 2:S1-S62. (PubMed)
6. Beckmann J, Lips KS. The non-neuronal cholinergic system in health and disease. Pharmacology. 2013;92(5-6):286-302. (PubMed)
7. Noga AA, Vance DE. A gender-specific role for phosphatidylethanolamine N-methyltransferase-derived phosphatidylcholine in the regulation of plasma high density and very low density lipoproteins in mice. J Biol Chem. 2003;278(24):21851-21859. (PubMed)
8. Noga AA, Zhao Y, Vance DE. An unexpected requirement for phosphatidylethanolamine N-methyltransferase in the secretion of very low density lipoproteins. J Biol Chem. 2002;277(44):42358-42365. (PubMed)
9. da Costa KA, Kozyreva OG, Song J, Galanko JA, Fischer LM, Zeisel SH. Common genetic polymorphisms affect the human requirement for the nutrient choline. Faseb J. 2006;20(9):1336-1344. (PubMed)
10. Pellanda H. Betaine homocysteine methyltransferase (BHMT)-dependent remethylation pathway in human healthy and tumoral liver. Clin Chem Lab Med. 2013;51(3):617-621. (PubMed)
11. Gerhard GT, Duell PB. Homocysteine and atherosclerosis. Curr Opin Lipidol. 1999;10(5):417-428. (PubMed)
12. Zeisel SH. Choline. In: Ross A, Caballero B, Cousins R, Tucker K, Ziegler T, eds. Modern Nutrition in Health and Disease. 11th ed: Lippincott Williams & Wilkins; 2014:416-426.
13. Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10(11):656-665. (PubMed)
14. Zeisel SH, Blusztajn JK. Choline and human nutrition. Annu Rev Nutr. 1994;14:269-296. (PubMed)
15. da Costa KA, Niculescu MD, Craciunescu CN, Fischer LM, Zeisel SH. Choline deficiency increases lymphocyte apoptosis and DNA damage in humans. Am J Clin Nutr. 2006;84(1):88-94. (PubMed)
16. Rolo AP, Teodoro JS, Palmeira CM. Role of oxidative stress in the pathogenesis of nonalcoholic steatohepatitis. Free Radic Biol Med. 2012;52(1):59-69. (PubMed)
17. Fischer LM, daCosta KA, Kwock L, et al. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am J Clin Nutr. 2007;85(5):1275-1285. (PubMed)
18. Fischer LM, da Costa KA, Kwock L, Galanko J, Zeisel SH. Dietary choline requirements of women: effects of estrogen and genetic variation. Am J Clin Nutr. 2010;92(5):1113-1119. (PubMed)
19. Resseguie M, Song J, Niculescu MD, da Costa KA, Randall TA, Zeisel SH. Phosphatidylethanolamine N-methyltransferase (PEMT) gene expression is induced by estrogen in human and mouse primary hepatocytes. Faseb J. 2007;21(10):2622-2632. (PubMed)
20. da Costa KA, Corbin KD, Niculescu MD, Galanko JA, Zeisel SH. Identification of new genetic polymorphisms that alter the dietary requirement for choline and vary in their distribution across ethnic and racial groups. FASEB J. 2014;28(7):2970-2978. (PubMed)
21. Kohlmeier M, da Costa KA, Fischer LM, Zeisel SH. Genetic variation of folate-mediated one-carbon transfer pathway predicts susceptibility to choline deficiency in humans. Proc Natl Acad Sci U S A. 2005;102(44):16025-16030. (PubMed)
22. Spencer MD, Hamp TJ, Reid RW, Fischer LM, Zeisel SH, Fodor AA. Association between composition of the human gastrointestinal microbiome and development of fatty liver with choline deficiency. Gastroenterology. 2011;140(3):976-986. (PubMed)
23. Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575-1584. (PubMed)
24. Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011;472(7341):57-63. (PubMed)
25. Korsmo HW, Jiang X, Caudill MA. Choline: exploring the growing science on its benefits for moms and babies. Nutrients. 2019;11(8). (PubMed)
26. Wallace TC, Blusztajn JK, Caudill MA, et al. Choline: the underconsumed and underappreciated essential nutrient. Nutr Today. 2018;53(6):240-253. (PubMed)
27. Bernhard W, Shunova A, Machann J, et al. Resolution of severe hepatosteatosis in a cystic fibrosis patient with multifactorial choline deficiency: A case report. Nutrition. 2021;89:111348. (PubMed)
28. Grothe J, Riethmuller J, Tschurtz SM, et al. Plasma phosphatidylcholine alterations in cystic fibrosis patients: impaired metabolism and correlation with lung function and inflammation. Cell Physiol Biochem. 2015;35(4):1437-1453. (PubMed)
29. Bernhard W, Poets CF, Franz AR. Choline and choline-related nutrients in regular and preterm infant growth. Eur J Nutr. 2019;58(3):931-945. (PubMed)
30. Jacob RA, Jenden DJ, Allman-Farinelli MA, Swendseid ME. Folate nutriture alters choline status of women and men fed low choline diets. J Nutr. 1999;129(3):712-717. (PubMed)
31. Kim YI, Miller JW, da Costa KA, et al. Severe folate deficiency causes secondary depletion of choline and phosphocholine in rat liver. J Nutr. 1994;124(11):2197-2203. (PubMed)
32. Food and Nutrition Board, Institute of Medicine. Choline. Dietary Reference Intakes: Thiamin, Riboflavin, Niacin, Vitamin B-6, Vitamin B-12, Pantothenic Acid, Biotin, and Choline. Washington D.C.: National Academy Press; 1998:390-422. (National Academy Press)
33. Ganz AB, Klatt KC, Caudill MA. Common genetic variants alter metabolism and influence dietary choline requirements. Nutrients. 2017;9(8):252. (PubMed)
34. Ganz AB, Cohen VV, Swersky CC, et al. Genetic variation in choline-metabolizing enzymes alters choline metabolism in young women consuming choline intakes meeting current recommendations. Int J Mol Sci. 2017;18(2):837. (PubMed)
35. Zhou J, Austin RC. Contributions of hyperhomocysteinemia to atherosclerosis: Causal relationship and potential mechanisms. Biofactors. 2009;35(2):120-129. (PubMed)
36. Leach NV, Dronca E, Vesa SC, et al. Serum homocysteine levels, oxidative stress and cardiovascular risk in non-alcoholic steatohepatitis. Eur J Intern Med. 2014;25(8):762-767. (PubMed)
37. Olthof MR, Brink EJ, Katan MB, Verhoef P. Choline supplemented as phosphatidylcholine decreases fasting and postmethionine-loading plasma homocysteine concentrations in healthy men. Am J Clin Nutr. 2005;82(1):111-117. (PubMed)
38. Olthof MR, van Vliet T, Boelsma E, Verhoef P. Low dose betaine supplementation leads to immediate and long term lowering of plasma homocysteine in healthy men and women. J Nutr. 2003;133(12):4135-4138. (PubMed)
39. Schwab U, Torronen A, Toppinen L, et al. Betaine supplementation decreases plasma homocysteine concentrations but does not affect body weight, body composition, or resting energy expenditure in human subjects. Am J Clin Nutr. 2002;76(5):961-967. (PubMed)
40. Steenge GR, Verhoef P, Katan MB. Betaine supplementation lowers plasma homocysteine in healthy men and women. J Nutr. 2003;133(5):1291-1295. (PubMed)
41. Dalmeijer GW, Olthof MR, Verhoef P, Bots ML, van der Schouw YT. Prospective study on dietary intakes of folate, betaine, and choline and cardiovascular disease risk in women. Eur J Clin Nutr. 2008;62(3):386-394. (PubMed)
42. Millard HR, Musani SK, Dibaba DT, et al. Dietary choline and betaine; associations with subclinical markers of cardiovascular disease risk and incidence of CVD, coronary heart disease and stroke: the Jackson Heart Study. Eur J Nutr. 2018;57(1):51-60. (PubMed)
43. Zheng Y, Li Y, Rimm EB, et al. Dietary phosphatidylcholine and risk of all-cause and cardiovascular-specific mortality among US women and men. Am J Clin Nutr. 2016;104(1):173-180. (PubMed)
44. Yang JJ, Lipworth LP, Shu XO, et al. Associations of choline-related nutrients with cardiometabolic and all-cause mortality: results from 3 prospective cohort studies of blacks, whites, and Chinese. Am J Clin Nutr. 2020;111(3):644-656. (PubMed)
45. Nagata C, Wada K, Tamura T, et al. Choline and betaine intakes are not associated with cardiovascular disease mortality risk in Japanese men and women. J Nutr. 2015;145(8):1787-1792. (PubMed)
46. Bidulescu A, Chambless LE, Siega-Riz AM, Zeisel SH, Heiss G. Usual choline and betaine dietary intake and incident coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) study. BMC Cardiovasc Disord. 2007;7:20. (PubMed)
47. Bertoia ML, Pai JK, Cooke JP, et al. Plasma homocysteine, dietary B vitamins, betaine, and choline and risk of peripheral artery disease. Atherosclerosis. 2014;235(1):94-101. (PubMed)
48. Golzarand M, Mirmiran P, Azizi F. Association between dietary choline and betaine intake and 10.6-year cardiovascular disease in adults. Nutr J. 2022;21(1):1. (PubMed)
49. Lundberg P, Dudman NP, Kuchel PW, Wilcken DE. 1H NMR determination of urinary betaine in patients with premature vascular disease and mild homocysteinemia. Clin Chem. 1995;41(2):275-283. (PubMed)
50. Lever M, George PM, Elmslie JL, et al. Betaine and secondary events in an acute coronary syndrome cohort. PLoS One. 2012;7(5):e37883. (PubMed)
51. Konstantinova SV, Tell GS, Vollset SE, Nygard O, Bleie O, Ueland PM. Divergent associations of plasma choline and betaine with components of metabolic syndrome in middle age and elderly men and women. J Nutr. 2008;138(5):914-920. (PubMed)
52. Meyer KA, Benton TZ, Bennett BJ, et al. Microbiota-dependent metabolite trimethylamine N-oxide and coronary artery calcium in the coronary artery risk development in young adults study (CARDIA). J Am Heart Assoc. 2016;5(10). (PubMed)
53. Yu D, Shu XO, Xiang YB, et al. Higher dietary choline intake is associated with lower risk of nonalcoholic fatty liver in normal-weight Chinese women. J Nutr. 2014;144(12):2034-2040. (PubMed)
54. Guerrerio AL, Colvin RM, Schwartz AK, et al. Choline intake in a large cohort of patients with nonalcoholic fatty liver disease. Am J Clin Nutr. 2012;95(4):892-900. (PubMed)
55. Mazidi M, Katsiki N, Mikhailidis DP, Banach M. Adiposity may moderate the link between choline intake and non-alcoholic fatty liver disease. J Am Coll Nutr. 2019;38(7):633-639. (PubMed)
56. Talaulikar VS, Arulkumaran S. Folic acid in obstetric practice: a review. Obstet Gynecol Surv. 2011;66(4):240-247. (PubMed)
57. Czeizel AE, Dudas I, Vereczkey A, Banhidy F. Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients. 2013;5(11):4760-4775. (PubMed)
58. Eskes TK. Open or closed? A world of difference: a history of homocysteine research. Nutr Rev. 1998;56(8):236-244. (PubMed)
59. Shaw GM, Carmichael SL, Yang W, Selvin S, Schaffer DM. Periconceptional dietary intake of choline and betaine and neural tube defects in offspring. Am J Epidemiol. 2004;160(2):102-109. (PubMed)
60. Carmichael SL, Yang W, Shaw GM. Periconceptional nutrient intakes and risks of neural tube defects in California. Birth Defects Res A Clin Mol Teratol. 2010;88(8):670-678. (PubMed)
61. Chandler AL, Hobbs CA, Mosley BS, et al. Neural tube defects and maternal intake of micronutrients related to one-carbon metabolism or antioxidant activity. Birth Defects Res A Clin Mol Teratol. 2012;94(11):864-874. (PubMed)
62. Petersen JM, Parker SE, Crider KS, Tinker SC, Mitchell AA, Werler MM. One-carbon cofactor intake and risk of neural tube defects among women who meet folic acid recommendations: a multicenter case-control study. Am J Epidemiol. 2019;188(6):1136-1143. (PubMed)
63. Lavery AM, Brender JD, Zhao H, et al. Dietary intake of choline and neural tube defects in Mexican Americans. Birth Defects Res A Clin Mol Teratol. 2014;100(6):463-471. (PubMed)
64. Shaw GM, Finnell RH, Blom HJ, et al. Choline and risk of neural tube defects in a folate-fortified population. Epidemiology. 2009;20(5):714-719. (PubMed)
65. Mills JL, Fan R, Brody LC, et al. Maternal choline concentrations during pregnancy and choline-related genetic variants as risk factors for neural tube defects. Am J Clin Nutr. 2014;100(4):1069-1074. (PubMed)
66. Obeid R, Derbyshire E, Schon C. Association between maternal choline, fetal brain development, and child neurocognition: systematic review and meta-analysis of human studies. Adv Nutr. 2022;13(6):2445-2457. (PubMed)
67. Teather LA, Wurtman RJ. Dietary cytidine (5')-diphosphocholine supplementation protects against development of memory deficits in aging rats. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27(4):711-717. (PubMed)
68. Zeisel SH. Choline: critical role during fetal development and dietary requirements in adults. Annu Rev Nutr. 2006;26:229-250. (PubMed)
69. McCann JC, Hudes M, Ames BN. An overview of evidence for a causal relationship between dietary availability of choline during development and cognitive function in offspring. Neurosci Biobehav Rev. 2006;30(5):696-712. (PubMed)
70. Dauncey MJ. Nutrition, the brain and cognitive decline: insights from epigenetics. Eur J Clin Nutr. 2014;68(11):1179-1185. (PubMed)
71. Strain JJ, McSorley EM, van Wijngaarden E, et al. Choline status and neurodevelopmental outcomes at 5 years of age in the Seychelles Child Development Nutrition Study. Br J Nutr. 2013;110(2):330-336. (PubMed)
72. Villamor E, Rifas-Shiman SL, Gillman MW, Oken E. Maternal intake of methyl-donor nutrients and child cognition at 3 years of age. Paediatr Perinat Epidemiol. 2012;26(4):328-335. (PubMed)
73. Boeke CE, Gillman MW, Hughes MD, Rifas-Shiman SL, Villamor E, Oken E. Choline intake during pregnancy and child cognition at age 7 years. Am J Epidemiol. 2013;177(12):1338-1347. (PubMed)
74. Cheatham CL, Goldman BD, Fischer LM, da Costa KA, Reznick JS, Zeisel SH. Phosphatidylcholine supplementation in pregnant women consuming moderate-choline diets does not enhance infant cognitive function: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr. 2012;96(6):1465-1472. (PubMed)
75. Caudill MA, Strupp BJ, Muscalu L, Nevins JEH, Canfield RL. Maternal choline supplementation during the third trimester of pregnancy improves infant information processing speed: a randomized, double-blind, controlled feeding study. FASEB J. 2018;32(4):2172-2180. (PubMed)
76. Bahnfleth CL, Strupp BJ, Caudill MA, Canfield RL. Prenatal choline supplementation improves child sustained attention: A 7-year follow-up of a randomized controlled feeding trial. FASEB J. 2022;36(1):e22054. (PubMed)
77. Wang Z, Zhu W, Xing Y, Jia J, Tang Y. B vitamins and prevention of cognitive decline and incident dementia: a systematic review and meta-analysis. Nutr Rev. 2022;80(4):931-949. (PubMed)
78. Poly C, Massaro JM, Seshadri S, et al. The relation of dietary choline to cognitive performance and white-matter hyperintensity in the Framingham Offspring Cohort. Am J Clin Nutr. 2011;94(6):1584-1591. (PubMed)
79. Liu L, Qiao S, Zhuang L, et al. Choline intake correlates with cognitive performance among elder adults in the United States. Behav Neurol. 2021;2021:2962245. (PubMed)
80. Nurk E, Refsum H, Bjelland I, et al. Plasma free choline, betaine and cognitive performance: the Hordaland Health Study. Br J Nutr. 2013;109(3):511-519. (PubMed)
81. Eussen SJ, Ueland PM, Clarke R, et al. The association of betaine, homocysteine and related metabolites with cognitive function in Dutch elderly people. Br J Nutr. 2007;98(5):960-968. (PubMed)
82. Birks J. Cholinesterase inhibitors for Alzheimer's disease. Cochrane Database Syst Rev. 2006(1):CD005593. (PubMed)
83. Higgins JP, Flicker L. Lecithin for dementia and cognitive impairment. Cochrane Database Syst Rev. 2003(3):CD001015. (PubMed)
84. Bonvicini M, Travaglini S, Lelli D, Antonelli Incalzi R, Pedone C. Is citicoline effective in preventing and slowing down dementia?-a systematic review and a meta-analysis. Nutrients. 2023;15(2):386. (PubMed)
85. Gupta N, Yucel YH. Glaucoma as a neurodegenerative disease. Curr Opin Ophthalmol. 2007;18(2):110-114. (PubMed)
86. Hwang JS, Shin YJ. Role of choline in ocular diseases. Int J Mol Sci. 2021;22(9):4733. (PubMed)
87. Parisi V. Electrophysiological assessment of glaucomatous visual dysfunction during treatment with cytidine-5'-diphosphocholine (citicoline): a study of 8 years of follow-up. Doc Ophthalmol. 2005;110(1):91-102. (PubMed)
88. Parisi V, Coppola G, Ziccardi L, Gallinaro G, Falsini B. Cytidine-5'-diphosphocholine (Citicoline): a pilot study in patients with non-arteritic ischaemic optic neuropathy. Eur J Neurol. 2008;15(5):465-474. (PubMed)
89. Ottobelli L, Manni GL, Centofanti M, Iester M, Allevena F, Rossetti L. Citicoline oral solution in glaucoma: is there a role in slowing disease progression? Ophthalmologica. 2013;229(4):219-226. (PubMed)
90. Parisi V, Centofanti M, Ziccardi L, et al. Treatment with citicoline eye drops enhances retinal function and neural conduction along the visual pathways in open angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2015;253(8):1327-1340. (PubMed)
91. Rossetti L, Iester M, Tranchina L, et al. Can treatment with citicoline eyedrops reduce progression in glaucoma? The results of a randomized placebo-controlled clinical trial. J Glaucoma. 2020;29(7):513-520. (PubMed)
92. Grieb P. Neuroprotective properties of citicoline: facts, doubts and unresolved issues. CNS Drugs. 2014;28(3):185-193. (PubMed)
93. Putignano S, Gareri P, Castagna A, et al. Retrospective and observational study to assess the efficacy of citicoline in elderly patients suffering from stupor related to complex geriatric syndrome. Clin Interv Aging. 2012;7:113-118. (PubMed)
94. Davalos A, Alvarez-Sabin J, Castillo J, et al. Citicoline in the treatment of acute ischaemic stroke: an international, randomised, multicentre, placebo-controlled study (ICTUS trial). Lancet. 2012;380(9839):349-357. (PubMed)
95. Fioravanti M, Yanagi M. Cytidinediphosphocholine (CDP-choline) for cognitive and behavioural disturbances associated with chronic cerebral disorders in the elderly. Cochrane Database Syst Rev. 2005(2):CD000269. (PubMed)
96. Cotroneo AM, Castagna A, Putignano S, et al. Effectiveness and safety of citicoline in mild vascular cognitive impairment: the IDEALE study. Clin Interv Aging. 2013;8:131-137. (PubMed)
97. Alvarez-Sabin J, Ortega G, Jacas C, et al. Long-term treatment with citicoline may improve poststroke vascular cognitive impairment. Cerebrovasc Dis. 2013;35(2):146-154. (PubMed)
98. Clark WM, Williams BJ, Selzer KA, Zweifler RM, Sabounjian LA, Gammans RE. A randomized efficacy trial of citicoline in patients with acute ischemic stroke. Stroke. 1999;30(12):2592-2597. (PubMed)
99. Clark WM, Wechsler LR, Sabounjian LA, Schwiderski UE, Citicoline Stroke Study Group. A phase III randomized efficacy trial of 2000 mg citicoline in acute ischemic stroke patients. Neurology. 2001;57(9):1595-1602. (PubMed)
100. Agarwal A, Vishnu VY, Sharma J, et al. Citicoline in acute ischemic stroke: A randomized controlled trial. PLoS One. 2022;17(5):e0269224. (PubMed)
101. Secades JJ, Alvarez-Sabin J, Castillo J, et al. Citicoline for acute ischemic atroke: a systematic review and formal meta-analysis of randomized, double-blind, and placebo-controlled trials. J Stroke Cerebrovasc Dis. 2016;25(8):1984-1996. (PubMed)
102. Marti-Carvajal AJ, Valli C, Marti-Amarista CE, Sola I, Marti-Fabregas J, Bonfill Cosp X. Citicoline for treating people with acute ischemic stroke. Cochrane Database Syst Rev. 2020;8(8):CD013066. (PubMed)
103. Zafonte RD, Bagiella E, Ansel BM, et al. Effect of citicoline on functional and cognitive status among patients with traumatic brain injury: Citicoline Brain Injury Treatment Trial (COBRIT). JAMA. 2012;308(19):1993-2000. (PubMed)
104. Secades JJ, Trimmel H, Salazar B, Gonzalez JA. Citicoline for the management of patients with traumatic brain injury in the acute phase: a systematic review and meta-analysis. Life (Basel). 2023;13(2):369. (PubMed)
105. USDA, Agricultural Research Service, 2021. Usual Nutrient Intake from Food and Beverages, by Gender and Age, What We Eat in America, NHANES 2015-2018. Available http://www.ars.usda.gov/nea/bhnrc/fsrg.
106. Wallace TC, Fulgoni VL 3rd. Usual choline intakes are associated with egg and protein food consumption in the United States. Nutrients. 2017;9(8):839. (PubMed)
107. Wallace TC, Fulgoni VL, 3rd. Assessment of total choline intakes in the United States. J Am Coll Nutr. 2016;35(2):108-112. (PubMed)
108. Zeisel SH, Klatt KC, Caudill MA. Choline. Adv Nutr. 2018;9(1):58-60. (PubMed)
109. Chester DN, Goldman JD, Ahuja JK, Moshfegh AJ. Dietary Intakes of Choline: What We Eat in America, NHANES 2007-2008. Food Surveys Research Group Dietary Data Brief No. 9. October 2011. Available at: http://ars.usda.gov/Services/docs.htm?docid=19476.
110. Craig SA. Betaine in human nutrition. Am J Clin Nutr. 2004;80(3):539-549. (PubMed)
111. Koc H, Mar MH, Ranasinghe A, Swenberg JA, Zeisel SH. Quantitation of choline and its metabolites in tissues and foods by liquid chromatography/electrospray ionization-isotope dilution mass spectrometry. Anal Chem. 2002;74(18):4734-4740. (PubMed)
112. Hendler SS, Rorvik DR, eds. PDR for Nutritional Supplements. 2nd ed: Thomson Reuters; 2008.
113. US Department of Health and Human Services, National Institutes of Health, Office of Dietary Supplements. Dietary Supplement Label Database (DSLD). [Internet]. [cited 4/10/2023]. Available from: https://dsld.od.nih.gov/.
114. Busby MG, Fischer L, da Costa KA, Thompson D, Mar MH, Zeisel SH. Choline- and betaine-defined diets for use in clinical research and for the management of trimethylaminuria. J Am Diet Assoc. 2004;104(12):1836-1845. (PubMed)
115. Wang Z, Tang WH, Buffa JA, et al. Prognostic value of choline and betaine depends on intestinal microbiota-generated metabolite trimethylamine-N-oxide. Eur Heart J. 2014;35(14):904-910. (PubMed)
116. Heianza Y, Ma W, Manson JE, Rexrode KM, Qi L. Gut microbiota metabolites and risk of major adverse cardiovascular disease events and death: a systematic review and meta-analysis of prospective studies. J Am Heart Assoc. 2017;6(7):e004947. (PubMed)
117. Papandreou C, More M, Bellamine A. Trimethylamine N-oxide in relation to cardiometabolic health-cause or effect? Nutrients. 2020;12(5):1330. (PubMed)
118. Zeisel SH, Warrier M. Trimethylamine N-oxide, the microbiome, and heart and kidney disease. Annu Rev Nutr. 2017;37:157-181. (PubMed)
119. Gatarek P, Kaluzna-Czaplinska J. Trimethylamine N-oxide (TMAO) in human health. EXCLI J. 2021;20:301-319. (PubMed)
120. Canyelles M, Borras C, Rotllan N, Tondo M, Escola-Gil JC, Blanco-Vaca F. Gut microbiota-derived TMAO: a causal factor promoting atherosclerotic cardiovascular disease? Int J Mol Sci. 2023;24(3):1940. (PubMed)
121. Al-Obaide MAI, Singh R, Datta P, et al. Gut microbiota-dependent trimethylamine-N-oxide and serum biomarkers in patients with T2DM and advanced CKD. J Clin Med. 2017;6(9):86. (PubMed)
122. Zuo H, Svingen GFT, Tell GS, et al. Plasma concentrations and dietary intakes of choline and betaine in association with atrial fibrillation risk: results from 3 prospective cohorts with different health profiles. J Am Heart Assoc. 2018;7(8):e008190. (PubMed)
123. Diez-Ricote L, San-Cristobal R, Concejo MJ, et al. One-year longitudinal association between changes in dietary choline or betaine intake and cardiometabolic variables in the PREvencion con DIeta MEDiterranea-Plus (PREDIMED-Plus) trial. Am J Clin Nutr. 2022;116(6):1565-1579. (PubMed)
124. Hardwick RN, Clarke JD, Lake AD, et al. Increased susceptibility to methotrexate-induced toxicity in nonalcoholic steatohepatitis. Toxicol Sci. 2014;142(1):45-55. (PubMed)
125. Lever M, George PM, Slow S, et al. Fibrates may cause an abnormal urinary betaine loss which is associated with elevations in plasma homocysteine. Cardiovasc Drugs Ther. 2009;23(5):395-401. (PubMed)
126. Lever M, McEntyre CJ, George PM, et al. Extreme urinary betaine losses in type 2 diabetes combined with bezafibrate treatment are associated with losses of dimethylglycine and choline but not with increased losses of other osmolytes. Cardiovasc Drugs Ther. 2014;28(5):459-468. (PubMed)
127. Lever M, George PM, Slow S, et al. Fibrates plus betaine: a winning combination? N Z Med J. 2010;123(1324):74-78. (PubMed)
Essential Fatty Acids
Contents
Summary
- Linoleic acid (LA), an omega-6 fatty acid, and α-linolenic acid (ALA), an omega-3 fatty acid, are considered essential fatty acids because they cannot be synthesized by humans. (More information)
- The long-chain omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), can be synthesized from ALA, but due to low conversion efficiency, it is recommended to consume foods rich in EPA and DHA. (More information)
- Both omega-6 and omega-3 fatty acids are important structural components of cell membranes, serve as precursors to bioactive lipid mediators, and provide a source of energy. Long-chain omega-3 polyunsaturated fatty acids (PUFA in particular exert anti-inflammatory effects; it is recommended to increase their presence in the diet. (More information)
- Both dietary intake and endogenous metabolism influence whole body status of essential fatty acids. Genetic polymorphisms in fatty acid synthesizing enzymes can have a significant impact on fatty acid concentrations in the body. (More information)
- DHA supplementation during pregnancy may reduce the risks of early premature birth (birth before 34 weeks' gestation) and very low birth weight (<1.5 kg [<3 pounds 5 ounces]). (More information)
- DHA is important for visual and neurological development. However, supplementation with long-chain during pregnancy or early infancy appears to have no significant effect on children's visual acuity, neurodevelopment, and physical growth. (More information)
- Replacing saturated fat in the diet with omega-6 lowers total blood cholesterol; yet, randomized controlled trials have failed to demonstrate cardiovascular benefits in healthy people and people at risk for or with type 2 diabetes mellitus. Long-chain omega-3 PUFA supplementation may be useful to reduce mortality in patients with prevalent coronary heart disease (CHD) and in those with heart failure without preserved ventricular function. (More information)
- Increasing EPA and DHA intake may benefit individuals with type 2 diabetes mellitus, especially those with elevated serum triglycerides. However, evidence from large-scale randomized trials is insufficient to support the use of omega-3 PUFA supplements for cardiovascular disease prevention in those with type 2 diabetes. (More information)
- Observational studies have found fish intake to be associated with lower risks of cognitive deterioration and Alzheimer’s disease, but it is not yet clear whether supplementation with marine-derived omega-3 PUFA can help prevent cognitive decline. (More information)
- Several omega-3 formulations have been approved by the US Food and Drug Administration for the indication of treating severe hypertriglyceridemia. (More information)
- Although omega-3 PUFA deficiency may not be uncommon in neurodevelopmental and neuropsychiatric disorders, there is little evidence to suggest that supplementation may be a beneficial adjunct in the management of affected individuals. (More information)
- The Food and Nutrition Board of the US Institute of Medicine (now the National Academy of Medicine) established adequate intakes (AI) for omega-6 and omega-3 fatty acids. (More information)
Introduction
Omega-6 and omega-3 fatty acids are polyunsaturated fatty acids (PUFA), meaning they contain more than one cis double bond (1). In all omega-6 (ω6 or n-6) fatty acids, the first double bond is located between the sixth and seventh carbon atom from the methyl end of the fatty acid. Likewise, all omega-3 fatty acids (ω3 or n-3) have at least one double bond between the third and fourth carbon atom counting from the methyl end of the fatty acid. Scientific abbreviations for fatty acids tell the reader something about their chemical structure. For example, the scientific abbreviation for α-linolenic acid (ALA) is 18:3n-3. The first part (18:3) tells the reader that ALA is an 18-carbon fatty acid with three double bonds, while the second part (n-3) tells the reader that the first double bond is in the n-3 position, which defines this fatty acid as an omega-3 (Figures 1a & b). Double bonds introduce kinks in the hydrocarbon chain that influence the structure and physical properties of the fatty acid molecule (Figure 1c).
Although humans and other mammals can synthesize saturated fatty acids and some monounsaturated fatty acids from carbon groups in carbohydrates and proteins, they lack the delta (Δ) 12 and Δ15 desaturase enzymes necessary to insert a cis double bond at the n-6 or the n-3 position of a fatty acid (1). Consequently, omega-6 and omega-3 fatty acids are essential nutrients. The parent fatty acid of the omega-6 series is linoleic acid (LA; 18:2n-6), and the parent fatty acid of the omega-3 series is ALA (Figure 2 and Table 1). Humans can synthesize long-chain (20 carbons or more) omega-6 fatty acids, such as dihomo-γ-linolenic acid (DGLA; 20:3n-6) and arachidonic acid (AA; 20:4n-6), from LA and long-chain omega-3 fatty acids, such as eicosapentaenoic acid (EPA; 20:5n-3) and docosahexaenoic acid (DHA; 22:6n-3), from ALA (see Metabolism and Bioavailability).
[Figure 1a and 1b - Click to Enlarge] [Figure 1c - Click to Enlarge]
Metabolism and Bioavailability
Prior to absorption in the small intestine, fatty acids must be hydrolyzed from dietary fats (triglycerides and phospholipids) by pancreatic enzymes (2). Bile salts must also be present in the small intestine to allow for the incorporation of fatty acids and other fat digestion products into mixed micelles. Fat absorption from mixed micelles occurs throughout the small intestine and is 85%-95% efficient under normal conditions.
Concentrations of fatty acids in blood (i.e., whole blood, plasma, serum, and red blood cells) reflect both dietary intake and biological processes (3). Humans can synthesize longer omega-6 and omega-3 fatty acids from the essential fatty acids linoleic acid (LA) and α-linolenic acid (ALA), respectively, through a series of desaturation (addition of a double bond between two carbon atoms) and elongation (addition of two carbon atoms) reactions (Figure 3) (4, 5). LA and ALA compete for the same elongase and desaturase enzymes in the synthesis of longer polyunsaturated fatty acids (PUFA), such as arachidonic acid (AA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA).
Studies of ALA metabolism in healthy young men indicated that approximately 8% of dietary ALA was converted to EPA and 0%-4% was converted to docosahexaenoic acid (DHA) (6). In healthy young women, approximately 21% of dietary ALA was converted to EPA and 9% was converted to DHA (7). The better capacity to generate long-chain PUFA from ALA in young women compared to men is related to the effects of estrogen (8, 9). Although only the essentiality of ALA is recognized because it cannot be synthesized de novo by humans, the relatively low rate of ALA conversion into EPA and DHA suggests that these long-chain omega-3 PUFA may be considered conditionally essential nutrients.
In addition to gender differences, genetic variability in enzymes involved in fatty acid metabolism influences one’s ability to generate long-chain PUFA. Two key enzymes in fatty acid metabolism are delta 6 desaturase (FADS2) and delta 5 desaturase (FADS1) (Figure 3) (10). Two common haplotypes (a cluster of polymorphisms) in the FADS genes differ dramatically in their ability to generate long-chain PUFA: haplotype D is associated with increased FADS activity (both FADS1 and FADS2) and higher conversion rate of fatty acid precursors (LA and ALA) to long-chain PUFA (EPA, GLA, DHA, and AA) (11). These FADS polymorphisms are relatively common in the population and may explain up to 30% of the variability in blood concentrations of omega-3 and omega-6 fatty acids among individuals (3).
Finally, DHA can be retro-converted to EPA and DPA at a low basal rate and following supplementation (Figure 3) (12). After supplementing omnivores (n=8) and vegetarians (n=12) for six weeks with an EPA-free preparation of DHA (1.62 g/day), EPA, DPA, and DHA concentrations increased in serum and platelet phospholipids (13). Based on the measured changes, the estimated percent retroconversion of DHA to EPA was 7.4%-11.4% (based on serum phospholipid data) and 12.3%-13.8% (based on platelet phospholipid data), with no significant difference between omnivores and vegetarians. Due to this nontrivial retroconversion efficiency, DHA supplementation may represent an alternative to fish oil to increase blood and tissue concentrations of EPA, DPA, and DHA (see Supplements) (5).
Biological Activities
Membrane structure and function
Omega-6 and omega-3 PUFA are important structural components of cell membranes. When incorporated into phospholipids, they affect cell membrane properties, such as fluidity, flexibility, permeability, and the activity of membrane-bound enzymes and cell-signaling pathways (14, 15). In addition to endogenous metabolism, dietary consumption of fatty acids can modify the composition and molecular structure of cellular membranes. Thus, increasing omega-3 fatty acid intake increases the omega-3 content of red blood cells, immune cells (16), atherosclerotic plaques (17), cardiac tissue (18), and other cell types throughout the body.
DHA is selectively incorporated into retinal cell membranes and postsynaptic neuronal cell membranes, suggesting it plays important roles in vision and nervous system function. In fact, DHA represents the predominant PUFA in the retina and neuronal cells (19).
Vision
DHA is found at very high concentrations in the cell membranes of the retina; the retina conserves and recycles DHA even when omega-3 fatty acid intake is low (20). Animal studies indicate that DHA is required for the normal development and function of the retina. Moreover, these studies suggest that there is a critical period during retinal development when inadequate DHA will result in permanent abnormalities in retinal function. Research indicates that DHA plays an important role in the regeneration of the visual pigment rhodopsin, which plays a critical role in the visual transduction system that converts light hitting the retina to visual images in the brain (21).
Nervous system
The phospholipids of the brain's gray matter contain high proportions of long-chain PUFA, suggesting they are important to central nervous system function (22). AA stimulates glucose uptake by cortical astrocytes, meaning that it is important for energy metabolism (23). AA and DHA also increase the release of acetylcholine, which enhances synaptic plasticity and memory, thereby improving learning abilities (24). Although trials of PUFA supplementation during pregnancy and/or early infancy failed to show cognitive improvements in offspring (see Disease Prevention), the availability of omega-3 and omega-6 fatty acids to the fetus and infants is essential for the growth of their brain and development of brain functions. There is compelling evidence to suggest that PUFA are essential to neuronal growth and synapse formation, and for appropriate neurotransmission (reviewed in 25).
Synthesis of lipid mediators
Oxylipins
Oxylipins are potent chemical messengers derived from PUFA. They play critical roles in immune and inflammatory responses. The most common oxylipins are eicosanoids that encompass numerous bioactive lipid mediators derived from 20-carbon ("eicosa-") AA. Following stimulation by hormones, cytokines, and other stimuli, PUFA bound to membrane phospholipids are released from cell membranes and become substrates for dodecanoid, eicosanoid, and docosanoid production. Oxylipin synthesis relies primarily on three families of enzymes: cyclooxygenases (COX), lipoxygenases (LOX), and cytochrome p450 mono-oxygenases (P450s) (26). From C18-C22 precursors, COX enzymes produce prostaglandins, prostacyclins, and thromboxanes (collectively known as prostanoids); LOX produces leukotrienes and hydroxy fatty acids; and P450s produce hydroxyeicosatetraenoic acids ("HETEs") and epoxides (Figure 4).
Physiological responses to AA-derived eicosanoids differ from responses to EPA-derived eicosanoids. In general, EPA is a poor substrate for eicosanoid production and EPA-derives eicosanoids are less potent inducers of inflammation, blood vessel constriction, and coagulation than eicosanoids derived from AA (19, 27).
Nonetheless, it is an oversimplification to label all AA-derived eicosanoids as pro-inflammatory. AA-derived prostaglandins induce inflammation but also inhibit pro-inflammatory leukotrienes and cytokines and induce anti-inflammatory lipoxins, thereby modulating the intensity and duration of the inflammatory response via negative feedback (Figure 4) (17).
Pro-resolving mediators
A separate class of PUFA-derived bioactive lipids, specialized pro-resolving mediators (SPMs), has been more recently identified (reviewed in 28). These molecules function as local mediators of the resolution phase of inflammation, actively turning off the inflammatory response. SPMs are derived from both omega-6 and omega-3 PUFA (Figure 4) (29). The S-series of SPMs results from the LOX-mediated oxygenation of EPA and DHA, giving rise to S-resolvins, S-protectins, and S-maresins. A second class of SPMs, the R-series, is generated from the aspirin-dependent acetylation of COX-2 and subsequent generation of aspirin-triggered SPMs from AA, EPA, and DHA. It appears that these mediators may explain many of the anti-inflammatory actions of omega-3 fatty acids that have been described (16, 30).
Isoprostanes
Isoprostanes are prostaglandin-like compounds that are formed by non-enzymatic, free radical-induced oxidation of any PUFA with three or more double bonds (Figure 4) (26). Because they are produced upon exposure to free radicals, isoprostanes are often used as markers for oxidative stress. In contrast to prostanoids, isoprostanes are synthesized from esterified PUFA precursors and remain bound to the membrane phospholipid until cleaved by PLA2 and released into circulation. In addition to being used as markers of oxidative stress, isoprostanes may also function as inflammatory mediators, exerting both pro- and anti-inflammatory effects (26).
Regulation of gene expression
PUFA are pleiotropic regulators of cell function. They can regulate gene expression directly by interacting with transcription factors or indirectly by influencing membrane lipid composition and cell signaling pathways.
The results of cell culture and animal studies indicate that omega-6 and omega-3 fatty acids can modulate the expression of a number of genes, including those involved with fatty acid metabolism and inflammation (31, 32). Omega-6 and omega-3 fatty acids regulate gene expression by interacting with specific transcription factors, such as peroxisome proliferator-activated receptors (PPARs) (33). In many cases, PUFA act like hydrophobic hormones (e.g., steroid hormones) to control gene expression and bind directly to receptors like PPARs. These ligand-activated receptors then bind to the promoters of genes and function to increase/decrease transcription.
In other cases, PUFA regulate the abundance of transcription factors inside the cell's nucleus (14). Two examples include NFκB and SREBP-1. NFκB is a transcription factor involved in regulating the expression of multiple genes involved in inflammation. Omega-3 PUFA suppress NFκB nuclear content, thus inhibiting the production of inflammatory eicosanoids and cytokines. SREBP-1 is a major transcription factor controlling fatty acid synthesis, both de novo lipogenesis and PUFA synthesis. Dietary PUFA can suppress SREBP-1, which decreases the expression of enzymes involved in fatty acid synthesis and PUFA synthesis. In this way, dietary PUFA function as feedback inhibitors of all fatty acid synthesis.
By altering cell membrane fluidity, fatty acids can interfere with the activity of membrane receptor systems and thus indirectly influence signaling pathways and gene expression (34).
Deficiency
Essential fatty acid deficiency
Clinical signs of essential fatty acid deficiency include a dry scaly rash, decreased growth in infants and children, increased susceptibility to infection, and poor wound healing (35). Omega-3, omega-6, and omega-9 fatty acids compete for the same desaturase enzymes. The desaturase enzymes show preference for the different series of fatty acids in the following order: omega-3 > omega-6 > omega-9. Consequently, synthesis of the omega-9 fatty acid eicosatrienoic acid (20:3n-9, mead acid, or 5,8,11-eicosatrienoic acid) increases only when dietary intakes of omega-3 and omega-6 fatty acids are very low; therefore, mead acid is one marker of essential fatty acid deficiency (36). A plasma eicosatrienoic acid:arachidonic acid (triene:tetraene) ratio greater than 0.2 is generally considered indicative of essential fatty acid deficiency (35, 37). In patients who were given total parenteral nutrition containing fat-free, glucose-amino acid mixtures, biochemical signs of essential fatty acid deficiency developed in as little as 7 to 10 days (38). In these cases, the continuous glucose infusion resulted in high circulating insulin concentrations, which inhibited the release of essential fatty acids stored in adipose tissue. When glucose-free amino acid solutions were used, parenteral nutrition up to 14 days did not result in biochemical signs of essential fatty acid deficiency. Essential fatty acid deficiency has also been found to occur in patients with chronic fat malabsorption (39) and in patients with cystic fibrosis (40). It has been proposed that essential fatty acid deficiency may play a role in the pathology of protein-energy malnutrition (36).
Omega-3 fatty acid deficiency
At least one case of isolated omega-3 fatty acid deficiency has been reported. A young girl who received intravenous lipid emulsions with very little ALA developed visual problems and sensory neuropathy; these conditions were resolved when she was administered an emulsion containing more ALA (41). Isolated omega-3 fatty acid deficiency does not result in increased plasma triene:tetraene ratios, and skin atrophy and dermatitis are absent (1). Plasma DHA concentrations decrease when omega-3 fatty acid intake is insufficient, but no accepted plasma omega-3 fatty acid or eicosanoid concentrations indicative of impaired health status have been defined (1). Studies in rodents have revealed significant impairment of n-3 PUFA deficiency on learning and memory (42, 43), prompting research in humans to assess the impact of omega-3 PUFA on cognitive development and cognitive decline (see Cognitive and visual development and Alzheimer's disease).
Omega-3 index
The omega-3 index is defined as the amount of EPA plus DHA in red blood cell membranes expressed as the percent of total red blood cell membrane fatty acids (44). The EPA + DHA content of red blood cell membranes correlates with that of cardiac muscle cells (45, 46), and several observational studies indicate that a lower omega-3 index is associated with an increased risk of coronary heart disease mortality (47). It is therefore proposed that the omega-3 index be used as a biomarker for cardiovascular disease risk, with suggested cutoffs as follows: high risk, <4%; intermediate risk, 4%-8%; and low risk, >8% (48).
Supplementation with EPA + DHA from fish oil capsules for approximately five months dose-dependently increased the omega-3 index in 115 healthy, young adults (ages, 20-45 years), validating the use of the omega-3 index as a biomarker of EPA + DHA intake (49). Before the omega-3 index can be used in routine clinical evaluation, however, clinical reference values in the population must be established (50). Additionally, fatty acid metabolism may be altered in certain disease states, potentially making the omega-3 index less relevant for some cardiovascular conditions (5).
Disease Prevention
Pregnancy and early childhood developmental outcomes
Supplementation during pregnancy
Effect on pregnancy-associated conditions and neonatal outcomes: The results of randomized controlled trials during pregnancy suggest that omega-3 polyunsaturated fatty acid (PUFA) supplementation does not decrease the incidence of gestational diabetes and preeclampsia (51-54) but may result in modest increases in length of gestation, especially in women with low omega-3 fatty acid consumption. A 2006 meta-analysis of six randomized controlled trials in women with low-risk pregnancies found that omega-3 PUFA supplementation during pregnancy resulted in an increased length of pregnancy by 1.6 days (55). A 2007 meta-analysis of randomized controlled trials in women with high-risk pregnancies found that supplementation with long-chain PUFA did not affect pregnancy duration or the overall incidence of premature births (birth before 37 weeks' gestation) but decreased the incidence of early premature births (birth before 34 weeks' gestation; 2 trials, 291 participants) (56). Analyses of the secondary outcomes of the 2010 DHA to Optimize Mother-Infant Outcome (DOMInO) trial in 2,399 participants showed that supplementation with DHA-enriched fish oil capsules (800 mg/day of DHA and 100 mg/day of EPA) during pregnancy (from <21 gestational weeks until birth) reduced the risk of early premature birth but increased the risk of obstetrical interventions like the need for induction or cesarean section, when compared to supplementation with DHA-free vegetable oil capsules (57). A 2016 meta-analysis of trials found evidence to suggest that omega-3 PUFA supplementation during pregnancy reduced the overall risk of prematurity and the risk of early premature births, increased gestational age at delivery and birth weight, and had no effect on the risks of perinatal death and low Apgar scores at 1 minute post birth (58). A dose-response analysis found a continuous reduction of the risks of early premature birth (birth before 34 weeks' gestation) and very low birth weight (birth weight <1,500 g) with daily doses of DHA supplement up to at least 600 mg during pregnancy (59). There is currently limited evidence to support a role for omega-3 supplementation in the prevention of recurrent intrauterine growth restriction (IUGR) (60) or recurrent preterm birth (61).
Effect on children's cognitive and visual development: The effect of maternal omega-3 long-chain PUFA supplementation on early childhood cognitive and visual development was summarized in a 2013 systematic review and meta-analysis (62). Included in this assessment were 11 randomized controlled trials (a total of 5,272 participants) that supplemented maternal diet with omega-3 long-chain PUFA during pregnancy or both pregnancy and lactation. Results regarding visual outcomes (eight trials) could not be pooled together due to variability in assessments; overall, four of six trials had null findings and the remaining two trials had very high rates of attrition. Cognitive outcomes (nine trials) included the Developmental Standard Score (DSS; in infants, toddlers, and preschoolers) or Intelligence Quotient (IQ; in children) and other aspects of neurodevelopment, such as language, behavior, and motor function. No differences were found between DHA and control groups for cognition measured with standardized psychometric scales in infants (<12 months), toddlers (12-24 months), and school-aged children (5-12 years); preschool children (2-5 years) in the DHA treatment group had a substantially higher DSS score compared to controls. The authors noted that many of the trials of long-chain PUFA supplementation in pregnancy had methodological weaknesses (e.g., high rates of attrition, small sample sizes, high risk of bias, multiple comparisons), limiting the confidence and interpretation of the pooled results. Of note, a seven-year follow-up of the DOMInO trial is currently underway to assess the effect of DHA supplementation during pregnancy on child IQ and various measures of cognitive development (e.g., executive functioning, memory, language) (63).
Effect on children’s body composition: The follow-up of 1,531 children whose mothers were randomized to supplemental DHA (800 mg/day) or a control during the second half of pregnancy in the DOMInO trial showed no effect of maternal DHA supplementation on the body mass index (BMI)-for-age z score and percentage of body fat of their children at three and five years of age (64). Measures of insulin resistance in 5-year-old children were unexpectedly higher in children whose mothers were in the DHA group than in those whose mothers were in the control group (64). Further analyses conducted in a subset of children (252) at age seven years again showed no effect of DHA supplementation on BMI z score, percentage of body fat, height, weight, and waist/hip circumference (65). Current evidence from 10 randomized controlled trials primarily conducted in high-income countries (all but one) suggests no influence of maternal supplementation with long-chain PUFA on the body composition and anthropometry of the offspring (66).
Effect on children's risk of allergies and asthma: A 2018 meta-analysis of randomized controlled trials in 2,047 children followed for six months to 16 years found a 19% lower risk of wheezing and/or asthma with maternal supplementation of omega-3 PUFA (primarily EPA and DHA) from as early as the 20th week of gestation until delivery (67). However, there was no effect of prenatal supplementation when the analysis was restricted to the three trials that reported on the incidence of childhood asthma only (67). Another meta-analysis of nine trials in 3,637 children, including three trials in which maternal supplementation with omega-3 PUFA continued after birth, found no effect of prenatal supplements on the risk of any allergy (three trials), the risk of wheeze and/or asthma (seven trials), the risk of eczema (six trials), the development of allergic rhinitis (two trials), and the risk of food allergy (three trials) in children (68). There was, however, some evidence to suggest that prenatal supplementation could lower the incidence of sensitization to specific allergens, namely egg (three trials; -46%) and peanut (two trials; -38%) (68).
Supplementation to breast-feeding mothers
A 2015 systematic review and meta-analysis summarized the results of eight randomized controlled trials that examined the effect of maternal supplementation with long-chain PUFA during either pregnancy and lactation or lactation only on the development and growth of their infants over the first two years of life and beyond (69). All studies were conducted in high-income countries. No differences between long-chain PUFA supplementation and control were observed in terms of language development, intelligence or problem-solving ability, psychomotor development, and anthropometric measurements (weight, length/height, head circumference, BMI, fat mass distribution) (69).
Supplementation in infants
The last trimester of pregnancy and first six months of postnatal life are critical periods for the accumulation of DHA in the brain and retina (70). Human milk contains a mixture of saturated fatty acids (~46%), monounsaturated fatty acids (~41%), omega-6 PUFA (~12%), and omega-3 PUFA (~1.3%) (71). Although human milk contains DHA in addition to ALA and EPA, ALA was the only omega-3 fatty acid present in conventional infant formulas until the year 2001. Although infants can synthesize DHA from ALA, they generally cannot synthesize enough to prevent declines in plasma and cellular DHA concentrations without additional dietary intake. Therefore, it was proposed that infant formulas be supplemented with enough DHA to bring plasma and cellular DHA concentrations of formula-fed infants up to those of breast-fed infants (72).
All infants: Although formulas enriched with DHA raise plasma and red blood cell DHA concentrations in preterm and term infants, the results of randomized controlled trials examining measures of visual acuity and neurological development in infants fed formula with or without added DHA have been mixed. For instance, a 2012 meta-analysis of randomized controlled trials (12 trials, 1,902 infants) comparing long-chain PUFA-supplemented and unsupplemented formula, started within one month of birth, found no effect of long-chain PUFA supplementation on infant cognition assessed at approximately one year of age (73). A lack of effect was observed regardless of the dose of long-chain PUFA or the prematurity status of the infant. With respect to visual acuity, a 2013 meta-analysis of randomized controlled trials (19 trials, 1,949 infants) found a beneficial effect of long-chain PUFA-supplemented formula, started within one month of birth, on infant visual acuity up to 12 months of age (74). Notably, two different types of visual acuity assessment were evaluated in the meta-analysis. Visual acuity assessed by using the Visually Evoked Potential (10 trials, 852 infants) showed a significant positive effect of long-chain PUFA-supplemented formula at 2, 4, and 12 months of age. When assessed by the Behavioral Method (12 trials, 1,095 infants), a significant benefit of long-chain PUFA-supplemented formula on visual acuity was found only at the age of two months. No moderating effects of dose or prematurity status were observed.
Preterm infants: A few trials have been specifically conducted in preterm infants. This is the case of the DHA for the Improvement of Neurodevelopmental Outcome (DINO) trial that initially enrolled 657 very preterm infants (born <33 gestational weeks) in five Australian hospitals (75). The aim of the trial was to examine the effect of enteral feeds with either high DHA (1% of total fatty acids) or standard DHA level (0.3% of total fatty acids) to preterm infants from age 2 to 4 days of life until term's corrected age (mean duration, 9.4 weeks) on their mental and psychomotor development, assessed at 18 months' and 7 years' corrected ages. At the 18-month follow-up, there was no difference in mean Mental Development Index (MDI) and Psychomotor Development Index (PDI) test scores between high-DHA and standard-DHA groups; yet, better MDI scores in girls fed high-DHA versus those fed standard-DHA feeds were reported in subgroup analyses (75). Post-hoc analyses also suggested fewer cases with delayed mental development among girls and infants weighing <1,250 kg at birth in the high- versus standard-DHA group (75). Follow-up at 7 years’ corrected age showed no difference between groups in measures of IQ and cognitive development, including attention, short-term verbal memory and learning ability, executive functioning, visual perception, and academic achievement (76). A 2016 systematic review of 17 trials found little evidence to suggest that supplementing preterm infants with long-chain PUFA (primarily AA and DHA) improved measures of visual acuity, neurodevelopment, and physical growth during infancy (77).
Cardiovascular disease
Omega-6 fatty acids
Linoleic acid (LA) is the most abundant dietary PUFA and accounts for approximately 90% of dietary omega-6 PUFA intake (78).
Observational studies: A pooled analysis of 13 prospective cohort studies, encompassing 310,602 individuals and 12,479 coronary heart disease (CHD) events (of which resulted in 5,882 CHD deaths) over follow-up periods of 5.3 to 30 years, found higher LA intakes to be associated with a 15% lower risk of CHD events and a 21% lower risk of CHD mortality (79). A dose-response analysis found that replacing 5% of energy from saturated fatty acids with LA was associated with a 9% lower risk of coronary events and a 13% lower risk of coronary deaths (79). A 2019 meta-analysis of 30 prospective cohort studies in 68,659 participants found that individuals in the highest versus lowest quintile of LA concentrations in tissues (primarily blood compartments) had a 23% lower risk of cardiovascular mortality (80). No associations were found between LA concentrations in tissues and the risks of CHD, ischemic stroke, or total cardiovascular disease (80).
Randomized controlled trials: Taking into consideration the results from four randomized controlled trials (81-85) that compared the effects of diets either high in saturated fatty acids or PUFA over at least two years, a 2016 systematic review and presidential advisory from the American Heart Association concluded that lowering saturated fat intake and replacing it with vegetable oil rich in PUFA (primarily soybean oil) could reduce the risk of CHD by 29% (86). Of note, these trials were conducted in the 1960s and 1970s, when the use of cholesterol-lowering drug statin was not widespread and the saturated fat content in diets was higher; all but one trial (84, 85) were in men with diagnosed cardiovascular disease (CVD). Among these four trials, the Oslo Diet-Heart Study (83) increased both omega-3 and omega-6 PUFA intake, and the Finnish Mental Hospital Study (84, 85) used a cross-over design — both trials were excluded from a Cochrane systematic review of 19 randomized controlled trials that examined the effect of increasing omega-6 PUFA intake on CVD outcomes (87). Of these 19 trials, seven assessed the effect of supplemental γ-linolenic acid (GLA) and 12 assessed the effect of substituting dietary LA for saturated or monounsaturated fatty acids. The pooled analysis of studies showed no effect of increasing omega-6 intake on the risks of CHD or CVD events, major adverse cardiac and cerebrovascular events, myocardial infarction (MI), stroke, CVD mortality, or all-cause mortality (low-quality evidence) (87). Moreover, many trials that examined the effect of replacing saturated fatty acids with mostly omega-6 PUFA may not have been adequately controlled. For example, in some trials, only the experimental group (the high omega-6 PUFA group) received dietary advice regarding more than just replacing saturated fatty acids by omega-3 PUFA, e.g., to avoid dietary sources of trans fatty acids and processed foods, to consume more whole-plant foods, to lower sugar consumption, to increase consumption of fish and shellfish, which could have biased the results (88). Additionally, a recent meta-analysis of trials with low risk of bias (i.e., free of differences between intervention and control groups other than those under examination) showed no evidence of an effect of substituting omega-6 PUFA for saturated fatty acids on the risks of major CHD events (MI and sudden death), total CHD events, CHD mortality, and all-cause mortality (88).
Yet, replacing dietary saturated fatty acids with omega-6 PUFA was consistently found to lower total blood cholesterol concentrations (87, 89). In fact, LA has been shown to be the most potent fatty acid for lowering total cholesterol when substituted for dietary saturated fatty acids (90). The potential mechanisms by which LA reduces blood cholesterol include (1) the upregulation of LDL receptor and redistribution of LDL-cholesterol from plasma to tissue, (2) the increase in bile acid production and cholesterol catabolism, and (3) the decreased VLDL-to-LDL conversion (91). However, if substituting omega-6 PUFA for saturated fatty acids can reduce blood cholesterol, the most recent systematic reviews and meta-analyses have failed to find evidence of clinical cardiovascular benefits (see above) (87, 88, 92).
Omega-3 fatty acids
Observational studies: A meta-analysis of 17 prospective and two retrospective cohort studies in 45,637 generally healthy participants found that circulating concentrations of α-linolenic acid (ALA) and longer chain omega-3 PUFA (i.e., eicosapentaenoic acid [EPA], docosapentaenoic acid [DPA], docosahexaenoic acid [DHA]) were inversely associated with the risk of fatal coronary heart disease (CHD) (93).
Several observational studies also examined the relationship between dietary ALA intake and the risk of CHD. A 2018 meta-analysis of 14 prospective cohort studies in a total of 345,202 participants free of cardiovascular disease (CVD) evaluated the risk of composite CHD outcomes (combining different CHD events) and fatal CHD in relation to dietary consumption of ALA (94). Overall, the pooled analysis found a 9% lower risk of composite CHD outcomes and a 15% lower risk of fatal CHD with higher ALA exposure (94). Further, a number of prospective cohort studies have examined the consumption of fish, rich in long-chain omega-3 PUFA (mainly EPA and DHA), in relation to various cardiovascular events and mortality. A 2018 review of the evidence and advisory from the American Heart Association concluded that seafood intake was associated with modestly lower risks of CHD, ischemic stroke, and sudden cardiac death, and noted a greater benefit when intake went from zero to one or two seafood meals per week and when seafood was substituted for less healthy options like processed meat (95). In contrast, recently published meta-analyses of prospective cohort studies found little evidence of inverse associations between fish consumption and either CHD or stroke (96, 97). Higher fish consumption was found to be associated with lower risks of myocardial infarction (MI) (98) and congestive heart failure (96). In addition, one meta-analysis of 12 prospective cohort studies found a 6% lower risk of all-cause mortality with the highest versus lowest level of fish consumption (99). Yet, another meta-analysis found no association between fish intake and all-cause mortality but a 4% lower risk of CVD mortality for each 20-g/day increment in fish intake (100).
The potential cardiovascular benefit of seafood consumption appears to be tightly linked to the type of seafood (e.g., fatty or lean fish), the way it is prepared (e.g., baked, broiled, or fried), the presence of toxic metals and environmental contaminants, and the habitual level of consumption (high versus low) — these factors may be confounding the results reported in observational studies and pooled analyses (95). Although seafood is a good source of long-chain omega-3 PUFA, health benefits associated with fish consumption could be attributed to the presence of other nutritional factors (e.g., micronutrients and high-quality protein) and that seafood consumption is usually a marker of higher socioeconomic status, as well as healthy lifestyles (101, 102).
Randomized controlled trials: A 2018 Cochrane systematic review assessed the evidence for a cardioprotective effect of ALA and long-chain omega-3 PUFA in individuals either at low or high risk of CVD (103). Moderate-to-high quality evidence from randomized controlled trials (of at least 12 months) suggested no effect of omega-3 PUFA (either supplemented, enriched in meals, or advised to be consumed) on the risk of CHD events, CVD events, arrhythmia, stroke, CHD mortality, CVD mortality, or all-cause mortality. There was also no evidence of an effect on secondary outcomes, including major adverse cerebrovascular or cardiovascular events, MI, sudden cardiac death, angina pectoris, heart failure, revascularization, peripheral arterial disease, and acute coronary syndrome (103). A 2017 review and advisory from the American Heart Association found no evidence to suggest a benefit of long-chain omega-3 PUFA supplementation for the prevention of cardiovascular mortality in patients with or at risk of type 2 diabetes mellitus, the prevention of CHD in patients with atherosclerotic disease (e.g., with prior stroke, peripheral vascular disease, diabetes, hypercholesterolemia), the prevention of stroke in patients with or without a history of stroke, and the prevention of atrial fibrillation in patients with prior atrial fibrillation or in those undergoing cardiac surgery (104). There was some evidence to suggest that supplementation with long-chain omega-3 PUFA in patients with prior clinical CHD might reduce the risk of CHD death, possibly because of a reduction in the risk of ischemia-induced sudden cardiac death (104).
Hypertriglyceridemia (borderline high: serum triglycerides 150-199 mg/dL; high: serum triglycerides >200 mg/dL) is an independent risk factor for cardiovascular disease (105). Numerous controlled clinical trials have demonstrated that increasing intakes of EPA and DHA significantly lower serum triglyceride concentrations (103). The triglyceride-lowering effects of EPA and DHA increase with dose (106), but clinically meaningful reductions in serum triglyceride concentrations have been demonstrated at doses of 2 g/day of EPA + DHA (107). Although long-chain omega-3 PUFA can reduce triglyceride concentrations, they have no effect on total cholesterol, LDL-cholesterol, or HDL-cholesterol in blood (103). Of note, the mechanisms by which long-chain omega-3 PUFA supplements may reduce CHD death are unlikely to involve a lowering of triglycerides as doses used in the studies (~1 g/day) were generally too low (104). Some studies in cell culture indicated that long-chain omega-3 PUFA may decrease the excitability of cardiac muscle cells (myocytes) by modulating ion channel conductance, which would be consistent with anti-arrhythmic effects observed in animal models (see also Hypertriglyceridemia) (108, 109).
Summary
Replacing dietary saturated fatty acids with omega-6 PUFA lowers total blood cholesterol, yet there is no convincing evidence of an effect of omega-6 PUFA on the risk of major CVD events. Although evidence supports the adoption of a heart-healthy dietary pattern that includes two servings of seafood per week (95), supplementation with long-chain omega-3 fatty acids is unlikely to result in cardiovascular benefits in generally healthy people with a low CVD risk or in individuals at risk of or with type 2 diabetes mellitus (104). In its recommendations regarding omega-3 fatty acids and cardiovascular disease (see Intake Recommendations), the American Heart Association indicates that long-chain omega-3 PUFA supplementation may be useful to reduce mortality in patients with prevalent CHD (e.g., who suffered a recent MI) and in those with heart failure without preserved ventricular function (104).
Cardiometabolic risk factors in individuals with diabetes mellitus
Type 2 diabetes mellitus: Cardiovascular disease is the leading cause of death in individuals with diabetes mellitus. The dyslipidemia typically associated with diabetes is characterized by a combination of hypertriglyceridemia (serum triglycerides >200 mg/dL), low HDL-cholesterol, and abnormal LDL-cholesterol (110). Lipid-lowering therapy to normalize diabetic dyslipidemia and reduce cardiovascular risk includes lifestyle modification and medications — particularly the use of cholesterol-lowering statins (111, 112). Additionally, achieving glucose control in people with type 2 diabetes has been shown to decrease the occurrence of major microvascular and macrovascular events (113).
A 2014 meta-analysis of 19 randomized controlled trials, including 24,788 individuals with either impaired glucose metabolism or type 2 diabetes mellitus, found that long-chain omega-3 PUFA supplementation (doses, 360-10,000 mg/day; for 6 weeks to 6 years) lowered serum triglyceride concentrations by 0.25 mmol/L but had no substantial effect on total cholesterol, LDL-cholesterol, or HDL-cholesterol (114). There was also no significant effect on HbA1c, fasting glucose, blood pressure, heart rate, or a measure of endothelial function. Four trials that lasted over a year reported on cardiovascular outcomes, including mortality. The pooled analysis of these trials found no effect of supplementation with omega-3 PUFA on the risk of major cardiovascular events, cardiovascular mortality, all-cause mortality, or a composite endpoint of all-cause mortality and hospitalization for a cardiovascular cause. It is worth noting that two of these trials — the Alpha Omega Trial (115) and the ORIGIN trial (116) — included a high proportion of participants who took cardiovascular medications (i.e., cholesterol-lowering statins) (114). Another meta-analysis of 45 randomized controlled trials in 2,674 participants with type 2 diabetes found that supplementation with omega-3 (400-1,800 mg/day for 2 weeks to 2 years) led to small decreases in blood concentrations of triglycerides, VLDL-triglycerides, LDL-cholesterol, and vLDL-cholesterol (117). There was no evidence of an effect on total cholesterol, HDL-cholesterol, non-esterified fatty acids, apolipoprotein-A1, and apolipoprotein-B. There was a reduction in circulating concentrations of pro-inflammatory cytokines, TNF-α and IL-6, in response to omega-3 supplementation, yet not of C-reactive protein (CRP) — a marker of low-grade inflammation. Omega-3 PUFA supplementation had no effect on systolic or diastolic blood pressure. Finally, a small decrease in HbA1c was reported in response to supplemental omega-3 fatty acids, yet there was no effect on other indicators of glycemic control, especially fasting glucose, fasting insulin, connecting (C-) peptide, and a measure of insulin resistance (117).
Lifestyle changes involving dietary modifications, such as the substitution of healthy fats (mono- and poly-unsaturated fatty acids) for saturated and trans fats, are recommended to reduce the risk of cardiovascular disease in people with type 2 diabetes mellitus (118). In their most recent updated recommendations on the prevention of cardiovascular disease in adults with type 2 diabetes, the American Diabetes Association and American Heart Association found insufficient evidence from large-scale randomized trials in individuals with type 2 diabetes to support the use of omega-3 fatty acid supplements (combined with a heart-healthy diet) in the prevention of cardiovascular events (118).
Gestational diabetes: Poor glycemic control during pregnancy, whether due to type 1 diabetes, type 2 diabetes, or gestational diabetes, increases the risk of fetal anomalies, preeclampsia, spontaneous abortion, stillbirth, macrosomia, neonatal hypoglycemia, and neonatal hyperbilirubinemia (119). Diabetes during pregnancy is also associated with a higher risk of metabolic disorders in offspring later in life (119). A team of investigators in Iran examined the effect of omega-3 PUFA supplementation during pregnancy, beginning at 24 to 28 weeks' gestation for six weeks, in women with gestational diabetes. Overall, there was evidence of beneficial effects of 1,000 mg/day of omega-3 alone (120) or together with vitamin E (121) or vitamin D (122) on markers of glucose homeostasis and, to a lesser extent, on markers of oxidative stress and inflammation and blood lipid profile. In one randomized, placebo-controlled trial in 60 women with gestational diabetes, supplementation with omega-3 fatty acids and vitamin E reduced the risk of neonatal hyperbilirubinemia yet had no effect on the rate of cesarean section, need for insulin therapy, maternal hospitalization, newborns' hospitalization, gestational age, birth size, and Apgar score (122).
Current recommendations by the American Diabetes Association for the management of gestational diabetes encourage the development of an individualized nutrition plan between a woman and a registered dietitian, highlighting the importance of the amount and type of carbohydrates in the diet (119). The use of omega-3 supplements in the management of gestational diabetes is not currently under consideration.
Type 2 diabetes mellitus
A meta-analysis of 13 randomized, controlled feeding trials that substituted plant-derived PUFA (primarily linoleic acid [LA]) for saturated fatty acids or carbohydrates for 3 to 16 weeks in generally healthy adults showed a decrease in fasting insulin concentration and insulin resistance but no effect on fasting glucose concentration (123). Most studies used a mixture of omega-3 and omega-6 PUFA in the form of plant-derived oils such that potential differences in effect between them could not be examined.
A meta-analysis of 20 prospective cohort studies conducted in 10 countries, in a total of 39,740 participants free from diabetes at baseline, examined biomarkers of omega-6 intake in relation to the risk of developing type 2 diabetes mellitus (124). LA ranged from 8.3% of total fatty acids in erythrocyte phospholipids to 54.5% in plasma cholesterol esters. The lowest percentage of arachidonic acid (AA) was found in adipose tissue (0.3%) and the highest in erythrocyte phospholipids (17.0%). The highest versus lowest concentration of LA markers in each compartment (phospholipids, plasma or serum, cholesterol esters) except adipose tissue was associated with a 35% lower risk of type 2 diabetes. In contrast, only AA in plasma or serum was inversely associated with the risk of type 2 diabetes (124). If LA concentration in blood and adipose tissue can provide an objective assessment of dietary LA intake (125), these results suggest that dietary LA may be important for glycemic control and diabetes prevention.
Metabolic syndrome
A 2019 meta-analysis of 13 observational (9 cross-sectional, 2 case-control, 1 nested case-control, and 1 prospective cohort; 36,542 participants) studies showed higher concentrations of omega-3 in blood and adipose tissue and higher level of omega-3 intake to be associated with a lower risk of metabolic syndrome (126). No association was found between tissue omega-6 concentration or dietary omega-6 intake level and the risk of metabolic syndrome (126).
Cognitive decline and Alzheimer's disease
Alzheimer’s disease is the most common cause of dementia in older adults (127). Alzheimer's disease is characterized by the formation of amyloid plaque in the brain and nerve cell degeneration. Disease symptoms, including memory loss and confusion, worsen over time (128).
Observational studies: Several observational studies have examined dietary fish and PUFA consumption in relation to risks of cognitive decline, dementia, and Alzheimer's disease. The pooled analysis of five large prospective cohort studies (Three-City Study, Nurses' Health Study, Women's Health Study, Chicago Health and Aging Project, and Rush Memory and Aging Project) that followed a total of 23,688 older (ages, ≥65 years) participants (88% women) for 3.9 to 9.1 years found slower rates of decline in episodic memory and global cognition with increasing fish intakes (129). Previous studies have suggested that the effect of fish or PUFA consumption on cognition may be dependent on apolipoprotein E (APOE) genotype (130, 131). Of three common APOE alleles (epsilon 2 [ε2], ε3, and ε4), the presence of the APOE ε4 (E4) allele has been associated with increased risk and earlier onset of Alzheimer's disease (132). It was found that long-chain omega-3 PUFA supplementation did not increase plasma omega-3 concentrations to the same extent in E4 carriers than in non-carriers (133) and that DHA metabolism differs in E4 carriers compared to non-carriers, with greater oxidation and lower plasma concentrations in E4 carriers (134). However, neither APOE genotype nor polymorphisms in 11 other genes associated with Alzheimer's disease were found to modify the inverse relationship between fish intake and risk of cognitive decline in the pooled analysis of the five cohorts (129).
In a recent meta-analysis of observational studies, each one-serving increase of fish intake per week was found to be associated with a 5% lower risk of dementia and a 7% lower risk of Alzheimer's disease (135). Dietary intake level of marine-derived DHA — but not blood DHA concentration — was also inversely associated with the risks of dementia and Alzheimer's disease; for instance, a 100 mg/day increment in dietary DHA intake was associated with lower risks of dementia (-14%) and Alzheimer's disease (-37%) (135). Results from two large cohort studies published after this dose-response meta-analysis showed blood DHA concentration to be positively associated with cognitive performance in adults (136, 137). Findings from preclinical studies suggest that long-chain omega-3 fatty acids may have neuroprotective effects, potentially through mitigating neuroinflammation, improving cerebral blood flow, and/or reducing amyloid aggregation (138).
Randomized controlled trials: A 2012 systematic review identified three randomized controlled trials that examined the effect of omega-3 supplementation on the risk of cognitive decline in cognitively healthy older or elderly adults (139). There was no evidence showing an effect of omega-3 on measures of cognitive functions in these clinical trials. In a more recent systematic review that identified seven trials conducted in cognitively healthy participants, the authors reported positive effects of long-chain omega-3 supplementation on measures of cognitive outcomes in all studies but the second longest and the two largest trials (140). Another seven trials examined the effect of long-chain omega-3 supplementation in individuals with mild cognitive impairment; all but three trials showed a significant benefit on measures of cognitive function or specific memory tasks (140). Yet, two trials that found no improvement in cognitive performance included omega-3 supplements in both intervention and control arms (141, 142).
Overall, the data favor a role for diets rich in long-chain omega-3 fatty acids in slowing cognitive decline, but larger trials with longer intervention periods may be necessary to see a consistent beneficial effect of omega-3 supplementation in older individuals with normal or declining cognitive functions.
Disease Treatment
Hypertriglyceridemia
About one-third of US adults have serum triglycerides >150 mg/dL, and 16% of US adults have serum triglycerides >200 mg/dL (143). The 2011 American Heart Association guidelines on triglyceride management recommended the use of marine-derived omega-3 fatty acid supplements (2-4 g/day of EPA plus DHA) under medical supervision to reduce triglyceride concentrations below 100 mg/dL (143). Hypertriglyceridemia can have various causes, such as inherited and acquired disorders of triglyceride metabolism, poor diet, and/or use of certain medications (143).
Several omega-3 fatty acid preparations have been approved by the US Food and Drug Administration for the treatment of hypertriglyceridemia (104). Out of the five currently available preparations, four contain ethyl esters of EPA and/or DHA and one contains long-chain omega-3 PUFA as free fatty acids (104). The Epanova for lowering very high triglycerides (EVOLVE) randomized controlled trial demonstrated that the omega-3 free fatty acid formulation (2-4 g/day for 12 weeks) effectively reduced triglycerides and other atherogenic factors, including vLDL-cholesterol and remnant-like cholesterol particles, when compared to olive oil (4 g/day) in patients with severe hypertriglyceridemia (serum triglycerides >500 mg/dL) (reviewed in 144). Omega-3 supplementation also decreased inflammation (as shown by a reduction in lipoprotein-associated phospholipase A2) and platelet activation (as shown by a reduction in circulating concentrations of arachidonic acid) (144, 145). This omega-3 formulation also proved to be effective in reducing persistent hypertriglyceridemia (serum triglycerides, 200-499 mg/dL) in patients treated with statins (cholesterol-lowering drugs) (146). Statin use has been found to effectively reduce triglyceride concentrations by about 5%-20% (147). However, a residual elevation in triglycerides and triglyceride-rich lipoprotein cholesterol may remain in a substantial fraction of patients treated with statins. Compared to 4 g/day of olive oil, omega-3 supplementation with 2 or 4 g/day for six weeks reduced triglycerides by 14.6% and 20.6% and non-HDL-cholesterol by 3.9% and 6.9%, respectively (146). The magnitude of these reductions in triglyceride and non-HDL-cholesterol concentrations was similar to what has been observed in other trials that examined the use of ethyl ester omega-3 supplements as add-ons to statin therapy (146, 148-150). A study is underway to assess the benefit of combining omega-3 fatty acids and statins on the risk of major cardiovascular events over a three- to five-year period in patients with hypertriglyceridemia (144, 151).
Nonalcoholic fatty liver disease
Often associated with metabolic disorders, nonalcoholic fatty liver disease (NAFLD) is a condition characterized by an excessive lipid accumulation in the liver (i.e., hepatosteatosis). NAFLD can progress to nonalcoholic steatohepatitis (NASH) in about one-third of the patients with NAFLD, thereby increasing the risk of cirrhosis and hepatocellular carcinoma (152, 153). An emerging feature of NAFLD is the decline in hepatic omega-3 and omega-6 PUFA with disease progression (154). Considering that C20-22 omega-3 PUFA can reduce fatty acid synthesis and inflammation, a possible therapeutic strategy would be to increase dietary intake of long-chain omega-3 PUFA. A 2018 meta-analysis of 18 randomized controlled trials in 1,424 participants with NAFLD found that omega-3 supplementation showed beneficial effects on liver fat, specific liver enzymatic activities, serum triglycerides, fasting glucose, and insulin resistance (155). However, there was no evidence of an effect on total cholesterol, LDL-cholesterol, HDL-cholesterol, fasting insulin, blood pressure, BMI, and waist circumference (155). Other recent meta-analyses have also reported that supplementation with long-chain omega-3 fatty acids from fish/seal oil (0.25-6.8 g/day for 3-25 months) improved hepatosteatosis and other metabolic disorders in both children and adults with NAFLD (reviewed in 153). Additional studies are needed to examine their efficacy in more severe cases of NASH.
Inflammatory diseases
Rheumatoid arthritis
A 2017 meta-analysis of 20 randomized controlled trials in 1,252 participants with rheumatoid arthritis assessed the efficacy of long-chain omega-3 PUFA supplementation on a series of clinical outcomes (156). Omega-3 supplementation (0.3-9.6 g/day) for 3 to 18 months reduced the number of tender joints (14 trials), as well as early morning stiffness (15 trials) and pain level (16 trials) compared to placebo. Blood concentrations of triglycerides (3 trials) and pro-inflammatory leukotriene B4 (5 trials) were also decreased with supplemental omega-3 PUFA (156). Another 2017 meta-analysis of 42 randomized controlled trials examined the effect of omega-3 supplementation (mainly as fish oil) on arthritic pain in patients diagnosed with different types of arthritis (157). Daily administration of marine-derived EPA (0.01-4.1 g) and DHA (0.01-2.7 g) for up to 18 months resulted in a reduction in patients’ reported pain (using a visual analog scale [VAS] for pain) in those suffering from rheumatoid arthritis (22 trials) and those with other types of arthritis (i.e., juvenile arthritis, psoriatic arthritis) or mixed diagnoses (3 trials), yet not in those with osteoarthritis (5 trials). The evidence of an effect of omega-3 supplements in patients with rheumatoid arthritis was deemed of moderate quality (157). In a 2017 systematic review of 18 trials, including 1,143 subjects with rheumatoid arthritis, only 4 of 18 placebo-controlled trials showed a benefit of omega-3 PUFA supplementation (2.2-3.6 g/day for 12-36 weeks) on pain level — reported by patients and/or assessed by physicians (158). In most trials, the use of medications (nonsteroidal anti-inflammatory drugs [NSAIDs] and/or disease-modifying anti-rheumatic drugs [DMARDs]) was continued throughout the intervention period. Results of a few trials suggested that omega-3 PUFA could spare the need for anti-inflammatory medications in some patients yet failed to show superiority of PUFA in pain management (159, 160).
The limited body of evidence that suggests potential benefits of omega-3 supplementation in rheumatoid arthritis treatment needs strengthening with data from larger studies conducted for longer intervention periods (157, 158).
Inflammatory bowel disease
Crohn's disease: A 2013 systematic review evaluated the efficacy of omega-3 supplementation in patients with Crohn's disease, considering the evidence base from both short-term (9 to 24 weeks) and long-term (1 year) trials (161). Among five trials that evaluated the efficacy of omega-3 supplementation on relapse rates, conflicting outcomes were reported. Most trials were limited by small sample sizes and short duration — up to three years may be necessary to see an effect on relapse rates given the natural relapsing-remitting course of the disease. The two largest and most recent trials (EPIC-1 and EPIC-2) showed no significant effect of omega-3 supplementation on indicators of Crohn's disease remission compared to placebo (162). Other systematic reviews of the literature reached similar conclusions (163-165). Three short-term trials showed positive effects of omega-3 supplementation on plasma biochemical parameters (e.g., reduced inflammatory cytokine expression, increased plasma EPA and DHA concentrations) compared to controls (161). In spite of its impact on biochemical changes in the short-term, however, the ability of omega-3 supplementation to maintain remission or effect clinically meaningful changes in Crohn's disease is not supported by the current evidence (164).
Ulcerative colitis: Seven randomized controlled trials of fish oil supplementation in patients with active ulcerative colitis reported significant improvement in at least one outcome measure, such as decreased corticosteroid use, improved disease activity scores, or improved histology scores (163). In patients with inactive ulcerative colitis, omega-3 supplementation had no effect on relapse rates compared to placebo in four separate trials (163, 165).
While no serious side effects were reported in any trials of fish oil supplementation for the maintenance or remission of inflammatory bowel disease, diarrhea and upper gastrointestinal symptoms occurred more frequently with omega-3 treatment (163-165).
Asthma
Inflammatory eicosanoids (leukotrienes) derived from arachidonic acid (AA; 20:4n-6) are thought to play an important role in the pathology of asthma (32). Because increasing omega-3 fatty acid intake has been found to decrease the formation of AA-derived leukotrienes, a number of clinical trials have examined the effects of long-chain omega-3 fatty acid supplementation on asthma. Although there is some evidence that omega-3 fatty acid supplementation can decrease the production of inflammatory mediators in asthmatic patients (166, 167), evidence that omega-3 fatty acid supplementation decreases the clinical severity of asthma in controlled trials has been inconsistent (168). Three systematic reviews of randomized controlled trials of long-chain omega-3 fatty acid supplementation in asthmatic adults and children found no consistent effects on clinical outcome measures, including pulmonary function tests, asthmatic symptoms, medication use, or bronchial hyperreactivity (169-171).
Immunoglobulin A nephropathy
Immunoglobulin A (IgA) nephropathy is a kidney disorder that results from the deposition of IgA in the glomeruli of the kidneys. The cause of IgA nephropathy is not clear, but progressive renal failure may eventually develop in 15%-40% of patients (172). Since glomerular IgA deposition results in increased production of inflammatory mediators, omega-3 fatty acid supplementation could potentially modulate the inflammatory response and preserve renal function.
A 2012 meta-analysis assessed the efficacy of omega-3 fatty acid supplementation on adult IgA nephropathy (173). Five randomized controlled trials were included in an analysis involving 239 patients (mean age, 37-41 years) who received placebo or supplemental EPA + DHA at doses of 1.4 to 5.1 g/day for 6 to 24 months. Compared with control groups, omega-3 supplementation had no significant effect on urine protein excretion or glomerular filtration rate. Only two trials measured changes in serum creatinine (a marker of renal function) and end-stage renal disease — omega-3 treatment had a beneficial effect on these two parameters in both trials. No adverse events associated with omega-3 supplementation were reported in any of the trials. A more recent review of the literature identified six trials showing evidence of omega-3 supplementation slowing IgA nephropathy disease progression and three trials reporting no effect (174). Additionally, preliminary data suggested that the potential synergistic actions of aspirin and long-chain omega-3 PUFAs might constitute a promising treatment option (168).
Neuropsychiatric disorders
Autism spectrum disorders
Autism spectrum disorders (ASD) refer to three neurodevelopmental disorders of variable severity, namely autism, Asperger syndrome, and pervasive development disorder. ASD are characterized by abnormal information processing in the brain due to alterations in the way nerve cells and their synapses connect and organize. ASD are thought to have a strong genetic basis, yet environmental factors including diet may play an important role. Given that omega-3 and omega-6 PUFA are necessary for neuronal growth and synapse formation (see Biological Activities), they may be of significant benefit in the prevention and/or management of ASD. This is supported by observations of PUFA abnormalities in blood of children with ASD, when compared to their peers with no neurodevelopmental disorders (175). A meta-analysis of case-control studies reported lower blood concentrations of DHA and EPA in children with ASD compared to typically developing children; yet, the ratio of total omega-6 to omega-3 fatty acids was similar between children with and without ASD symptoms (176). A systematic review by the same authors identified six randomized controlled trials that examined the effect of primarily long-chain omega-3 PUFA on ASD symptoms (176). All the studies included children; one study also included adults ≤28 years (177). Four trials used EPA (0.70-0.84 g/day) plus DHA (0.46-0.70 g/day) (178-181), one trial used DHA (0.24 g/day) plus AA (0.24 g/day) (177), and one trial only used only DHA (0.20 g/day) (182). A pooled analysis of four (177-180) of these trials, including a total of 107 participants, showed a small improvement in measures of social interaction and repetitive and restrictive interests and behaviors with long-chain PUFA supplementation for 6 to 16 weeks; however, there was no effect on measures of communication and ASD co-existing conditions, such as hyperactivity, irritability, sensory issues, and gastrointestinal symptoms (176). Two additional systematic reviews and meta-analyses, also published in 2017, identified the same set of trials. One meta-analysis suggested a benefit of long-chain PUFA on measures of lethargy and stereotypy but found no overall clinical improvement compared to placebo (183). The other meta-analysis suggested an improvement regarding lethargy yet a worsening of externalizing behavior and social skills in children supplemented with omega-3 PUFA (184).
The available evidence is based on few trials of small sample sizes and is thus too limited to draw firm conclusions regarding the potential benefit of long-chain PUFA supplementation in ASD management.
Major depression and bipolar disorder
Data from ecologic studies across different countries suggested an inverse association between seafood consumption and national rates of major depression (185) and bipolar disorder (186).
Several small studies have found omega-3 fatty acid concentrations to be lower in plasma (187-189) and adipose tissue (190) of individuals suffering from depression compared to controls. Although it is not known how omega-3 fatty acid intake affects the incidence of depression, modulation of neuronal signaling pathways and eicosanoid production have been proposed as possible mechanisms (191). There may be some benefit of omega-3 PUFA supplementation on depressive disorders, but it is difficult to compare studies and draw conclusions due to great heterogeneity among the trials (192, 193). Small sample sizes, lack of standardization of therapeutic doses, type of omega-3 PUFA administered, co-treatment with pharmacological agents, and diagnostic criteria vary among the trials. A 2012 systematic review of all published randomized controlled trials investigated the effect of omega-3 PUFA supplementation on the prevention and treatment of several types of depression and other neuropsychiatric disorders (192). With respect to major depression, most studies reported a positive effect of omega-3 supplements on depressive symptoms, though efficacy is still considered inconclusive given the great variability among trials. A few themes emerged from this review: more trials reported positive effect for omega-3 PUFA supplements as an adjunct to pharmacological treatment; in monotherapy trials, EPA alone was more effective than DHA alone; and in combination trials, positive effects were more likely if an EPA:DHA ratio of >1.5–2.0 was administered.
A 2014 meta-analysis grouped trials by type of diagnosis of depression (194). A positive effect of omega-3 supplementation was found in 11 trials in participants with a diagnosis of major depressive disorder (according to the Diagnostic and Statistical Manual of Mental Disorders [DSM] criteria). Omega-3 supplementation also appeared to be effective in the pooled analysis of eight trials in participants not formally diagnosed with major depressive disorder, i.e., adults with depressive symptoms despite ongoing treatment, untreated patients with mild-to-severe depressed mood, patients with a history of at least one major depressive episode, women with borderline personality disorder, patients with recurrent self-harm, and postmenopausal women with psychological distress and depressive symptoms. There was no mood improvement with omega-3 supplements in generally healthy adults experiencing depressive symptoms, as suggested by the pooled analysis of six trials (194).
Finally, a 2017 Cochrane systematic review and meta-analysis of 20 randomized controlled trials reported a small benefit of omega-3 supplementation on depressive symptoms when compared to placebo, yet the evidence was deemed of very low quality and the positive effect was judged likely to be biased and not clinically significant (195).
Unipolar depression and bipolar disorder are considered distinct psychiatric conditions, although major depression occurs in both. A 2016 meta-analysis of eight case-control studies that compared the PUFA composition of red blood cell membranes between patients with bipolar disorder and healthy subjects showed abnormally low red blood cell DHA concentrations with bipolar disorder (196). As with major depression, reviews of trials indicated that omega-3 supplementation may have a positive effect as an adjunct to therapy in patients with bipolar disorder (192, 194). Additionally, a 2016 randomized, placebo-controlled trial in 100 participants with bipolar disorder reported a reduction in the severity of manic episodes with daily supplementation of 1,000 mg omega-3 PUFA for three months (197).
While there is some promising evidence for the use of omega-3 fatty acids for major depression and bipolar disorder, additional trials that account for dietary omega-3 intake, changes in red blood cell PUFA concentrations, the ratio of EPA:DHA provided, and co-treatment with medications are necessary.
Schizophrenia
A 2013 meta-analysis of 18 studies compared the PUFA composition of red blood cell membranes in patients with schizophrenia to individuals without the disorder (198). The majority of studies investigated medicated patients, though the authors separated the analysis into three groups of patients at time of measurement in order to account for possible confounding from pharmacologic agents: antipsychotic-medicated, antipsychotic-naïve, and antipsychotic-free. Overall, decreased concentrations of DPA, DHA, and AA in red blood cell membranes were associated with the schizophrenic state. Several mechanisms may account for PUFA abnormalities in schizophrenia, such as altered lipid metabolism, increased oxidative stress, or changes in diet consequent to disease-related behavior.
The use of long-chain omega-3 fatty acid supplements to alleviate symptoms of schizophrenia or to mitigate adverse effects of antipsychotic medications has been investigated in a number of clinical trials (194, 199). In a recent randomized, placebo-controlled trial in 50 subjects with recent onset of schizophrenia who were medicated, daily supplementation with EPA (740 mg) and DHA (400 mg) reduced psychotic symptoms (assessed with the Brief Psychiatric Rating Scale) only in those who were not taking the anxiolytic, lorazepam (Ativan) (200). Overall, however, there was no effect of long-chain PUFA supplements on schizophrenia symptoms. Yet, given the high safety profile of fish oil supplements and some evidence of a positive effect of EPA supplementation in a subset of trials, some clinicians may consider EPA a useful adjunct to antipsychotic therapy in patients with schizophrenia.
Alzheimer's disease and dementia
Several mechanisms suggest that omega-3 PUFA supplementation may improve the cognitive performance of individuals with Alzheimer's disease and other types of dementia. In particular, the antioxidative and anti-inflammatory properties of these PUFA may help protect neurons, promote synaptic plasticity, and limit cellular death. The PUFA composition of the diet appears to influence blood cholesterol, which may play a role in the pathology of Alzheimer's disease. However, the current evidence from clinical trials is not supportive of omega-3 supplementation in the treatment of Alzheimer’s disease in humans. A 2016 Cochrane review identified three randomized, placebo-controlled trials in patients with Alzheimer's disease of mild-to-moderate severity (201). These trials compared daily supplementation with DHA (between 675 mg and 1,700 mg) and EPA (between 600 mg and 975 mg) to a placebo for 12 months (202, 203) or 18 months (204). Of note, the study by Quinn et al. (204) also included 4 mg/day of vitamin E (used as preservative — see also Nutrient interactions) in the intervention arm, and the study by Freund-Levi et al. (202) included DHA (900-1,100 mg/day) but no EPA. The pooled analysis of these trials showed no beneficial effect of omega-3 supplementation on measures of global and specific cognitive functions, measures of functional outcomes, and measures of dementia severity (201). There was no difference between intervention and placebo arms regarding the occurrence of adverse effects (201).
Sources
Food sources
Humans can synthesize arachidonic acid (AA) from linoleic acid (LA) and eicosapentaenoic acid (EPA) and docosapentaenoic acid (DHA) from α-linolenic acid (ALA) through a series of desaturation and elongation reactions. EPA and docosapentaenoic acid (DPA) are also obtained from the retroconversion of DHA (see Metabolism and Bioavailability). Due to low conversion efficiency, it is advised to obtain EPA and DHA from additional sources.
Omega-6 fatty acids
Linoleic acid (LA): Food sources of LA include vegetable oils, such as soybean, safflower, and corn oil; nuts; seeds; and some vegetables. Dietary surveys in the US indicate that the average adult intake of LA ranges from 17 to 20 g/day for men and 12 to 13 g/day for women (78). Some foods that are rich in LA are listed in Table 2.
| Food | Serving | Linoleic Acid (g) |
|---|---|---|
| Safflower oil | 1 tablespoon |
10.1
|
| Sunflower seeds, oil roasted | 1 ounce |
9.7
|
| Pine nuts | 1 ounce |
9.4
|
| Sunflower oil | 1 tablespoon |
8.9
|
| Corn oil | 1 tablespoon |
7.3
|
| Soybean oil | 1 tablespoon |
6.9
|
| Pecans, oil roasted | 1 ounce |
6.4
|
| Brazil nuts | 1 ounce |
5.8
|
| Sesame oil | 1 tablespoon |
5.6
|
Arachidonic acid: Animals, but not plants, can convert LA to AA. Therefore, AA is absent in vegetable oils and fats and present in small amounts in meat, poultry, and eggs.
Omega-3 fatty acids
α-Linolenic acid (ALA): Flaxseeds, walnuts, and their oils are among the richest dietary sources of ALA. Canola oil is also an excellent source of ALA. Dietary surveys in the US indicate that average adult intakes for ALA range from 1.8 to 2.0 g/day for men and from 1.4 to 1.5 g/day for women (78). Some foods that are rich in ALA are listed in Table 3.
| Food | Serving | α-Linolenic acid (g) |
|---|---|---|
| Flaxseed oil | 1 tablespoon |
7.3
|
| Chia seeds, dried | 1 ounce |
5.1
|
| Walnuts, English | 1 ounce |
2.6
|
| Flaxseeds, ground | 1 tablespoon |
1.6
|
| Walnut oil | 1 tablespoon |
1.4
|
| Canola oil | 1 tablespoon |
1.3
|
| Soybean oil | 1 tablespoon |
0.9
|
| Mustard oil | 1 tablespoon |
0.8
|
| Walnuts, black | 1 ounce |
0.6
|
| Tofu, firm | ½ cup |
0.2
|
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA): Dietary surveys in the US indicate that average adult intakes of EPA range from 0.03 to 0.06 g/day, and average adult intakes of DHA range from 0.05 to 0.10 g/day (78). Oily fish are the major dietary source of EPA and DHA; omega-3 fatty acid-enriched eggs are also available in the US. Some foods that are rich in EPA and DHA are listed in Table 4.
| Food | Serving | EPA (g) | DHA (g) |
Amount Providing 1 g of EPA + DHA |
|---|---|---|---|---|
| Herring, Pacific | 3 ounces* |
1.06
|
0.75
|
1.5 ounces
|
| Salmon, chinook | 3 ounces |
0.86
|
0.62
|
2 ounces
|
| Sardines, Pacific | 3 ounces |
0.45
|
0.74
|
2.5 ounces
|
| Salmon, Atlantic | 3 ounces |
0.28
|
0.95
|
2.5 ounces
|
| Oysters, Pacific | 3 ounces |
0.75
|
0.43
|
2.5 ounces
|
| Salmon, sockeye | 3 ounces |
0.45
|
0.60
|
3 ounces
|
| Trout, rainbow | 3 ounces |
0.40
|
0.44
|
3.5 ounces
|
| Tuna, canned, white | 3 ounces |
0.20
|
0.54
|
4 ounces
|
| Crab, Dungeness | 3 ounces |
0.24
|
0.10
|
9 ounces
|
| Tuna, canned, light | 3 ounces |
0.04
|
0.19
|
12 ounces
|
| *A three-ounce serving of fish is about the size of a deck of cards. | ||||
Supplements
Omega-6 fatty acids
Borage seed oil, evening primrose oil, and black currant seed oil are rich in γ-linolenic acid (GLA; 18:3n-6) and are often marketed as GLA or essential fatty acid (EFA) supplements (206).
Omega-3 fatty acids
Flaxseed oil (also known as flax oil or linseed oil) is available as an ALA supplement. A number of fish oils are marketed as omega-3 fatty acid supplements. The omega-3 fatty acids from natural fish oil are in the triglyceride form, often with only one of three attached fatty acids an omega-3; thus, up to 70% of fatty acids provided may be other types (3). Ethyl esters of EPA and DHA (ethyl-EPA and ethyl-DHA) are concentrated sources of long-chain omega-3 fatty acids that provide more EPA and DHA per gram of oil. Krill oil contains both EPA and DHA and is considered comparable to fish oil as a source of these long-chain PUFA (207). Cod liver oil is also a rich source of EPA and DHA, but some cod liver oil preparations may contain excessive amounts of preformed vitamin A (retinol) and vitamin D (206). DHA supplements derived from algal and fungal sources are also available. Because dietary DHA can be retroconverted to EPA and DPA in humans, DHA supplementation represents yet another alternative to fish oil supplements (see Metabolism and Bioavailability).
The content of EPA and DHA varies in each of these preparations, making it necessary to read product labels in order to determine the EPA and DHA levels provided by a particular supplement. All omega-3 fatty acid supplements are absorbed more efficiently with meals. Dividing one's daily dose into two or three smaller doses throughout the day will decrease the risk of gastrointestinal side effects (see Safety).
Infant formula
In 2001, the FDA began permitting the addition of DHA and AA to infant formula in the United States (208). Presently, manufacturers are not required to list the amounts of DHA and AA added to infant formula on the label. However, most infant formula manufacturers provide this information. The amounts added to formulas in the US range from 8 to 17 mg DHA/100 calories (5 fl oz) and from 16 to 34 mg AA/100 calories. For example, an infant drinking 20 fl oz of DHA-enriched formula daily would receive 32 to 68 mg/day of DHA and 64 to 136 mg/day of AA.
Safety
Adverse effects
γ-Linolenic acid (18:3n-6)
Supplemental γ-linolenic acid is generally well tolerated, and serious adverse side effects have not been observed at doses up to 2.8 g/day for 12 months (209). High doses of borage seed oil, evening primrose oil, or black currant seed oil may cause gastrointestinal upset, loose stools, or diarrhea (206). Because of case reports that supplementation with evening primrose oil induced seizure activity in people with undiagnosed temporal lobe epilepsy (210), people with a history of seizures or a seizure disorder are generally advised to avoid evening primrose oil and other γ-linolenic acid-rich oils (206).
α-Linolenic acid (18:3n-3)
Although flaxseed oil is generally well tolerated, high doses may cause loose stools or diarrhea (211). Allergic and anaphylactic reactions have been reported with flaxseed and flaxseed oil ingestion (212).
Eicosapentaenoic acid (20:5n-3) and docosahexaenoic acid (22:6n-3)
Serious adverse reactions have not been reported in those using fish oil or other EPA and DHA supplements. The most common adverse effect of fish oil or EPA and DHA supplements is a fishy aftertaste. Belching and heartburn have also been reported. Additionally, high doses may cause nausea and loose stools.
Potential for excessive bleeding: The potential for high omega-3 fatty acid intakes, especially EPA and DHA, to prolong bleeding times has been well studied and may play a role in the cardioprotective effects of omega-3 fatty acids. Although excessively long bleeding times and increased incidence of hemorrhagic stroke have been observed in Greenland Eskimos with very high intakes of EPA + DHA (6.5 g/day), it is not known whether high intakes of EPA and DHA are the only factor responsible for these observations (1). The US FDA has ruled that intakes up to 3 g/day of long-chain omega-3 fatty acids (EPA and DHA) are Generally Recognized As Safe (GRAS) for inclusion in the diet, and available evidence suggests that intakes less than 3 g/day are unlikely to result in clinically significant bleeding (107). Although the US Institute of Medicine did not establish a tolerable upper intake level (UL) for omega-3 fatty acids, caution was advised with the use of supplemental EPA and DHA, especially in those who are at increased risk of excessive bleeding (see Drug interactions and Nutrient interactions) (1, 206).
Potential for immune system suppression: Although the suppression of inflammatory responses resulting from increased omega-3 fatty acid intakes may benefit individuals with inflammatory or autoimmune diseases, anti-inflammatory doses of omega-3 fatty acids could decrease the potential of the immune system to destroy pathogens (213). Studies comparing measures of immune cell function outside the body (ex vivo) at baseline and after supplementing people with omega-3 fatty acids, mainly EPA and DHA, have demonstrated immunosuppressive effects at doses as low as 0.9 g/day for EPA and 0.6 g/day for DHA (1). Although it is not clear if these findings translate to impaired immune responses in vivo, caution should be observed when considering omega-3 fatty acid supplementation in individuals with compromised immune systems.
Potential other effects: Although fish oil supplements are unlikely to affect glucose homeostasis, people with diabetes mellitus who are considering fish oil supplements should inform their physician and be monitored if they choose to take them (206).
Infant formula
In early studies of DHA-enriched infant formula, EPA- and DHA-rich fish oil was used as a source of DHA. However, some preterm infants receiving fish oil-enriched formula had decreased plasma AA concentrations, which were associated with decreased weight (but not length and head circumference) (214, 215). This effect was attributed to the potential for high concentrations of EPA to interfere with the synthesis of AA, which is essential for normal growth. Consequently, EPA was removed and AA was added to DHA-enriched formula. Currently available infant formulas in the US contain only AA and DHA derived from algal or fungal sources, rather than fish oil. Randomized controlled trials have not found any adverse effects on growth in infants fed formulas enriched with AA and DHA for up to one year (216).
Pregnancy and lactation
The safety of supplemental omega-3 and omega-6 fatty acids, including borage seed oil, evening primrose oil, black currant seed oil, and flaxseed oil, has not been established in pregnant or lactating (breast-feeding) women (217). Studies of fish oil supplementation during pregnancy and lactation have not reported any serious adverse effects, but use of omega-6/omega-3 PUFA-containing supplements and fish oil supplements in pregnant or nursing women should be monitored by a physician (see Contaminants in fish and Contaminants in supplements) (206).
Contaminants in fish
Some species of fish may contain significant levels of methylmercury, polychlorinated biphenyls (PCBs), or other environmental contaminants (218). In general, larger predatory fish, such as swordfish, tend to contain the highest levels of these contaminants. Removing the skin, fat, and internal organs of the fish prior to cooking and allowing the fat to drain from the fish while it cooks will decrease exposure to a number of fat-soluble pollutants, such as PCBs (219). However, methylmercury is found throughout the muscle of fish, so these cooking precautions will not reduce exposure to methylmercury. Organic mercury compounds are toxic and excessive exposure can cause brain and kidney damage. The developing fetus, infants, and young children are especially vulnerable to the toxic effects of mercury on the brain. In order to limit their exposure to methylmercury, the US Food and Drug Administration (FDA) and Environmental Protection Agency have formulated joint recommendations for women who may become pregnant, pregnant women, breast-feeding women, and parents. These recommendations are presented in Table 5.
For more information about the FDA/Environmental Protection Agency advisory for pregnant women and parents of young children on eating fish, see their online brochure. More information about mercury levels in commercial fish and shellfish is available from the FDA.
Of note, the 2015-2020 Dietary Guidelines for Americans recommend the consumption of salmon, anchovies, herring, shad, sardines, Pacific oysters, trout, and Atlantic and Pacific mackerel (not king mackerel), which are higher in EPA and DHA and lower in methylmercury (220).
Contaminants in supplements
Although concerns have been raised regarding the potential for omega-3 fatty acid supplements derived from fish oil to contain methylmercury, PCBs, and dioxins, several independent laboratory analyses in the US have found commercially available omega-3 fatty acid supplements to be free of methylmercury, PCBs, and dioxins (221). The absence of methylmercury in omega-3 fatty acid supplements can be explained by the fact that mercury accumulates in the muscle, rather than the fat of fish (107). In general, fish body oils contain lower concentrations of PCBs and other fat-soluble contaminants than fish liver oils. Additionally, fish oils that have been more highly refined and deodorized contain lower concentrations of PCBs (222). Pyrrolizidine alkaloids, potentially hepatotoxic and carcinogenic compounds, are found in various parts of the borage plant. People who take borage oil supplements should use products that are certified free of unsaturated pyrrolizidine alkaloids (206).
| 1. Eat 8-12 ounces of a variety of fish a week |
|
| 2. Choose fish lower in mercury. |
|
| 3. Avoid 4 types of fish: tilefish from the Gulf of Mexico, shark, swordfish, and king mackerel. |
|
| 4. When eating fish you or others have caught from streams, rivers, and lakes, pay attention to fish advisories on those waterbodies. |
|
| 5. When adding more fish to your diet, be sure to stay within your calorie needs. |
Drug interactions
γ-Linolenic acid supplements, such as evening primrose oil or borage seed oil, may increase the risk of seizures in people on phenothiazines (neuroleptic agents), such as chlorpromazine (210). High doses of black currant seed oil, borage seed oil, evening primrose oil, flaxseed oil, and fish oil may inhibit platelet aggregation; therefore, these supplements should be used with caution in people on anticoagulant medications (206). In particular, people taking fish oil or long-chain omega-3 fatty acid (EPA and DHA) supplements in combination with anticoagulant drugs, including aspirin, clopidogrel (Plavix), dalteparin (Fragmin), dipyridamole (Persantine), enoxaparin (Lovenox), heparin, ticlopidine (Ticlid), and warfarin (Coumadin), should have their coagulation status monitored using a standardized prothrombin time assay (international normalized ratio [INR]). One small study found that 3 g/day or 6 g/day of fish oil did not affect INR values in 10 patients on warfarin over a four-week period (223). However, a case report described an individual who required a reduction of her warfarin dose when she doubled her fish oil dose from 1 g/day to 2 g/day (224).
Nutrient interactions
Vitamin E
Outside the body, PUFA become rancid (oxidized) more easily than saturated fatty acids. Fat-soluble antioxidants, such as vitamin E (α-tocopherol), play an important role in preventing the oxidation of PUFA. Inside the body, results of animal studies and limited data in humans suggest that the amount of vitamin E required to prevent lipid peroxidation increases with the amount of PUFA consumed (225). One widely used recommendation for vitamin E intake is 0.6 mg of α-tocopherol per gram of dietary PUFA. This recommendation was based on a small study in men and the ratio of α-tocopherol to LA in the US diet and has not been verified in more comprehensive studies. Although EPA and DHA are easily oxidized outside the body, it is presently unclear whether they are more susceptible to oxidative damage within the body (226). High vitamin E intakes have not been found to decrease biomarkers of oxidative damage when EPA and DHA intakes are increased (227, 228), but some experts believe that an increase in PUFA intake, particularly omega-3 PUFA intake, should be accompanied by an increase in vitamin E intake (1).
Intake Recommendations
US Institute of Medicine
The Food and Nutrition Board of the US Institute of Medicine (now the National Academy of Medicine) has established adequate intake (AI) for omega-6 and omega-3 fatty acids (Tables 6 and 7) (1).
| Life Stage | Age | Source | Males (g/day) | Females (g/day) |
|---|---|---|---|---|
| Infants | 0-6 months | Omega-6 PUFA* | 4.4 | 4.4 |
| Infants | 7-12 months | Omega-6 PUFA* | 4.6 | 4.6 |
| Children | 1-3 years | LA# | 7 | 7 |
| Children | 4-8 years | LA | 10 | 10 |
| Children | 9-13 years | LA | 12 | 10 |
| Adolescents | 14-18 years | LA | 16 | 11 |
| Adults | 19-50 years | LA | 17 | 12 |
| Adults | 51 years and older | LA | 14 | 11 |
| Pregnancy | all ages | LA | - | 13 |
| Breast-feeding | all ages | LA | - | 13 |
| *The various omega-6 polyunsaturated fatty acids (PUFA) present in human milk can contribute to the AI for infants. # LA, linoleic acid | ||||
| Life Stage | Age | Source | Males (g/day) | Females (g/day) |
|---|---|---|---|---|
| Infants | 0-6 months | ALA, EPA, DHA* |
0.5
|
0.5
|
| Infants | 7-12 months | ALA, EPA, DHA |
0.5
|
0.5
|
| Children | 1-3 years | ALA |
0.7
|
0.7
|
| Children | 4-8 years | ALA |
0.9
|
0.9
|
| Children | 9-13 years | ALA |
1.2
|
1.0
|
| Adolescents | 14-18 years | ALA |
1.6
|
1.1
|
| Adults | 19 years and older | ALA |
1.6
|
1.1
|
| Pregnancy | all ages | ALA |
-
|
1.4
|
| Breast-feeding | all ages | ALA |
-
|
1.3
|
| *All omega-3 polyunsaturated fatty acids present in human milk can contribute to the AI for infants. ALA, α-linolenic acid; EPA, eicosapentaenoic acid; DHA, docosahexaenoic acid. | ||||
Given the established health benefits of consuming at least two servings of oily fish per week, providing approximately 400 to 500 mg EPA + DHA, some researchers have proposed that the US Institute of Medicine (now the National Academy of Medicine) establish dietary reference intakes (DRIs) for EPA + DHA (27). For now, there are no DRIs for EPA and DHA specifically.
Because maternal dietary intake of long-chain PUFA determines the DHA status of the newborn, several expert panels in the US recommend that pregnant and lactating women consume at least 200 mg DHA per day, close to the amount recommended for adults in general (250 mg/day) (70, 229). The potential benefits associated with obtaining long-chain omega-3 fatty acids through moderate consumption of fish (e.g., 1-2 servings weekly) during pregnancy and lactation outweigh any risks of contaminant exposure, though fish with high concentrations of methylmercury should be avoided (218). For information about contaminants in fish and guidelines for fish consumption by women of childbearing age, see Contaminants in fish.
2015-2020 Dietary Guidelines for Americans
The 2015-2020 Dietary Guidelines provide recommendations for nutritional goals for linoleic acid and α-linolenic acid based on the DRIs (see Tables 6 and 7). Seafood, nuts, seeds, and oils, which are all part of healthy dietary patterns, provide essential fatty acids. The 2015-2020 Dietary Guidelines provide dietary recommendations regarding the amounts of these foods for those who choose to follow a healthy US-style eating pattern, a healthy Mediterranean-style eating pattern, or a healthy vegetarian eating pattern (Table 8).
| Food | Healthy Eating Patterns | ||
|---|---|---|---|
| US-style | Mediterranean-style | Vegetarian | |
| Seafood (oz-eq/week) | 8 | 15 | – |
|
Nuts, seeds, soy products (oz-eq/week)
|
5 | 5 | 7 |
| Oils (g/week) | 27 | 27 | 27 |
|
*Recommendations for total daily energy needs of 2,000 calories per day. Estimates of daily calorie needs according to age, gender, and physical activity can be found in the Appendix 2 of the ‘2015-2020 Dietary Guidelines for Americans’ report (220). Oz-eq, ounce-equivalent |
|||
American Heart Association recommendation
The American Heart Association recommends that people without documented coronary heart disease (CHD) eat a variety of fish (preferably oily) at least twice weekly (230). Two servings of oily fish provide approximately 500 mg of EPA plus DHA. Pregnant women and children should avoid fish that typically have higher levels of methylmercury (see Contaminants in fish). People with documented CHD and those with heart failure without preserved left ventricular function are advised to consume approximately 1 g/day of EPA + DHA preferably from oily fish, or to consider EPA + DHA supplements in consultation with a physician (104, 107). Patients who need to lower serum triglycerides may take 2 to 4 g/day of EPA + DHA supplements under a physician's care (see Hypertriglyceridemia).
International recommendations
Upon request of the European Commission, the European Food Safety Authority (EFSA) proposed adequate intakes (AI) for the essential fatty acids LA and ALA, as well as the long-chain omega-3 fatty acids EPA and DHA (231). EFSA recommends an LA intake of 4% of total energy and an ALA intake of 0.5% of total energy; an AI of 250 mg/day is recommended for EPA plus DHA (232). The European Food and Safety Authority (EFSA) recommends that pregnant and lactating women consume an additional 100 to 200 mg of preformed DHA on top of the 250 mg/day EPA plus DHA recommended for healthy adults (231).
For adults, the World Health Organization recommends an acceptable macronutrient distribution range (AMDR) for omega-6 fatty acid intake of 2.5%-9% of energy and for omega-3 fatty acid intake of 0.5%-2% of energy (233). Their AMDR for EPA plus DHA is 0.25 to 2 g/day (the upper level applying to secondary prevention of coronary heart disease).
The International Society for the Study of Fatty Acids and Lipids (ISSFAL) recommends healthy adults have an LA intake of 2% energy, an ALA intake of 0.7% energy, and a minimum of 500 mg/day of EPA plus DHA for cardiovascular health (234).
Linus Pauling Institute recommendation
The Linus Pauling Institute supports the AI for the essential fatty acids (see Tables 6 and 7) and recommends that generally healthy adults increase their intake of long-chain omega-3 fatty acids by eating fish twice weekly and consuming foods rich in ALA, such as walnuts, flaxseeds, and flaxseed or canola oil. If you don't regularly consume fish, consider taking a two-gram fish oil supplement several times a week. If you are prone to bleeding or take anticoagulant drugs, consult your physician.
Authors and Reviewers
Originally written in 2003 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in December 2005 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in April 2009 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in April 2014 by:
Giana Angelo, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in May 2019 by:
Barbara Delage, Ph.D.
Linus Pauling Institute
Oregon State University
Reviewed in June 2019 by:
Donald B. Jump, Ph.D.
Professor, School of Biological and Population Health Sciences
Principal Investigator, Linus Pauling Institute
Oregon State University
Copyright 2003-2025 Linus Pauling Institute
References
1. Food and Nutrition Board, Institute of Medicine. Dietary Fats: Total Fat and Fatty Acids. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, D.C.: National Academies Press; 2002:422-541. (The National Academies Press)
2. Lichtenstein A, Jones PJ. Lipids: Absorption and Transport. In: Erdman JWJ, Macdonald IA, Zeisel SH, eds. Present Knowledge in Nutrition. 10th ed: ILSI Wiley-Blackwell; 2012:118-131.
3. Davidson MH. Omega-3 fatty acids: new insights into the pharmacology and biology of docosahexaenoic acid, docosapentaenoic acid, and eicosapentaenoic acid. Curr Opin Lipidol. 2013;24(6):467-474. (PubMed)
4. Nakamura MT, Nara TY. Structure, function, and dietary regulation of delta6, delta5, and delta9 desaturases. Annu Rev Nutr. 2004;24:345-376. (PubMed)
5. Jump DB, Depner CM, Tripathy S. Omega-3 fatty acid supplementation and cardiovascular disease. J Lipid Res. 2012;53(12):2525-2545. (PubMed)
6. Burdge GC, Jones AE, Wootton SA. Eicosapentaenoic and docosapentaenoic acids are the principal products of α-linolenic acid metabolism in young men. Br J Nutr. 2002;88(4):355-364. (PubMed)
7. Burdge GC, Wootton SA. Conversion of α-linolenic acid to eicosapentaenoic, docosapentaenoic and docosahexaenoic acids in young women. Br J Nutr. 2002;88(4):411-420. (PubMed)
8. Burdge G. α-Linolenic acid metabolism in men and women: nutritional and biological implications. Curr Opin Clin Nutr Metab Care. 2004;7(2):137-144. (PubMed)
9. Giltay EJ, Gooren LJ, Toorians AW, Katan MB, Zock PL. Docosahexaenoic acid concentrations are higher in women than in men because of estrogenic effects. Am J Clin Nutr. 2004;80(5):1167-1174. (PubMed)
10. Tosi F, Sartori F, Guarini P, Olivieri O, Martinelli N. Delta-5 and delta-6 desaturases: crucial enzymes in polyunsaturated fatty acid-related pathways with pleiotropic influences in health and disease. Adv Exp Med Biol. 2014;824:61-81. (PubMed)
11. Ameur A, Enroth S, Johansson A, et al. Genetic adaptation of fatty-acid metabolism: a human-specific haplotype increasing the biosynthesis of long-chain omega-3 and omega-6 fatty acids. Am J Hum Genet. 2012;90(5):809-820. (PubMed)
12. Brossard N, Croset M, Pachiaudi C, Riou JP, Tayot JL, Lagarde M. Retroconversion and metabolism of [13C]22:6n-3 in humans and rats after intake of a single dose of [13C]22:6n-3-triacylglycerols. Am J Clin Nutr. 1996;64(4):577-586. (PubMed)
13. Conquer JA, Holub BJ. Dietary docosahexaenoic acid as a source of eicosapentaenoic acid in vegetarians and omnivores. Lipids. 1997;32(3):341-345. (PubMed)
14. Jump DB, Tripathy S, Depner CM. Fatty acid-regulated transcription factors in the liver. Ann Rev Nutr. 2013;33:249-269. (PubMed)
15. Stillwell W, Wassall SR. Docosahexaenoic acid: membrane properties of a unique fatty acid. Chem Phys Lipids. 2003;126(1):1-27. (PubMed)
16. Calder PC. n-3 fatty acids, inflammation and immunity: new mechanisms to explain old actions. Proc Nutr Soc. 2013;72(3):326-336. (PubMed)
17. Calder PC. Polyunsaturated fatty acids and inflammatory processes: New twists in an old tale. Biochimie. 2009;91(6):791-795. (PubMed)
18. Harris WS, Sands SA, Windsor SL, et al. Omega-3 fatty acids in cardiac biopsies from heart transplantation patients: correlation with erythrocytes and response to supplementation. Circulation. 2004;110(12):1645-1649. (PubMed)
19. Jump DB. The biochemistry of n-3 polyunsaturated fatty acids. J Biol Chem. 2002;277(11):8755-8758. (PubMed)
20. Jeffrey BG, Weisingerb HS, Neuringer M, Mitcheli DC. The role of docosahexaenoic acid in retinal function. Lipids. 2001;36(9):859-871. (PubMed)
21. SanGiovanni JP, Chew EY. The role of omega-3 long-chain polyunsaturated fatty acids in health and disease of the retina. Prog Retin Eye Res. 2005;24(1):87-138. (PubMed)
22. Innis SM. Dietary omega 3 fatty acids and the developing brain. Brain Res. 2008;1237:35-43. (PubMed)
23. Yu N, Martin JL, Stella N, Magistretti PJ. Arachidonic acid stimulates glucose uptake in cerebral cortical astrocytes. Proc Natl Acad Sci U S A. 1993;90(9):4042-4046. (PubMed)
24. Das UN, Fams. Long-chain polyunsaturated fatty acids in the growth and development of the brain and memory. Nutrition. 2003;19(1):62-65. (PubMed)
25. Das UN. Autism as a disorder of deficiency of brain-derived neurotrophic factor and altered metabolism of polyunsaturated fatty acids. Nutrition. 2013;29(10):1175-1185. (PubMed)
26. American Oil Chemists' Society. The AOCS Lipid Library. August 15, 2012. Available at: http://lipidlibrary.aocs.org/. Accessed 2/25/14.
27. Flock MR, Harris WS, Kris-Etherton PM. Long-chain omega-3 fatty acids: time to establish a dietary reference intake. Nutr Rev. 2013;71(10):692-707. (PubMed)
28. Serhan CN, Chiang N. Resolution phase lipid mediators of inflammation: agonists of resolution. Curr Opin Pharmacol. 2013;13(4):632-640. (PubMed)
29. Bannenberg G, Serhan CN. Specialized pro-resolving lipid mediators in the inflammatory response: An update. Biochim Biophys Acta. 2010;1801(12):1260-1273. (PubMed)
30. Nicolaou A, Mauro C, Urquhart P, Marelli-Berg F. Polyunsaturated Fatty Acid-Derived Lipid Mediators and T Cell Function. Front Immunol. 2014;5:75. (PubMed)
31. Price PT, Nelson CM, Clarke SD. Omega-3 polyunsaturated fatty acid regulation of gene expression. Curr Opin Lipidol. 2000;11(1):3-7. (PubMed)
32. Calder PC. Dietary modification of inflammation with lipids. Proc Nutr Soc. 2002;61(3):345-358. (PubMed)
33. Sampath H, Ntambi JM. Polyunsaturated fatty acid regulation of gene expression. Nutr Rev. 2004;62(9):333-339. (PubMed)
34. Shaikh SR. Biophysical and biochemical mechanisms by which dietary N-3 polyunsaturated fatty acids from fish oil disrupt membrane lipid rafts. J Nutr Biochem. 2012;23(2):101-105. (PubMed)
35. Jeppesen PB, Hoy CE, Mortensen PB. Essential fatty acid deficiency in patients receiving home parenteral nutrition. Am J Clin Nutr. 1998;68(1):126-133. (PubMed)
36. Smit EN, Muskiet FA, Boersma ER. The possible role of essential fatty acids in the pathophysiology of malnutrition: a review. Prostaglandins Leukot Essent Fatty Acids. 2004;71(4):241-250. (PubMed)
37. Mascioli EA, Lopes SM, Champagne C, Driscoll DF. Essential fatty acid deficiency and home total parenteral nutrition patients. Nutrition. 1996;12(4):245-249. (PubMed)
38. Stegink LD, Freeman JB, Wispe J, Connor WE. Absence of the biochemical symptoms of essential fatty acid deficiency in surgical patients undergoing protein sparing therapy. Am J Clin Nutr. 1977;30(3):388-393. (PubMed)
39. Jeppesen PB, Hoy CE, Mortensen PB. Deficiencies of essential fatty acids, vitamin A and E and changes in plasma lipoproteins in patients with reduced fat absorption or intestinal failure. Eur J Clin Nutr. 2000;54(8):632-642. (PubMed)
40. Lepage G, Levy E, Ronco N, Smith L, Galeano N, Roy CC. Direct transesterification of plasma fatty acids for the diagnosis of essential fatty acid deficiency in cystic fibrosis. J Lipid Res. 1989;30(10):1483-1490. (PubMed)
41. Holman RT, Johnson SB, Hatch TF. A case of human linolenic acid deficiency involving neurological abnormalities. Am J Clin Nutr. 1982;35(3):617-623. (PubMed)
42. Fedorova I, Hussein N, Baumann MH, Di Martino C, Salem N, Jr. An n-3 fatty acid deficiency impairs rat spatial learning in the Barnes maze. Behav Neurosci. 2009;123(1):196-205. (PubMed)
43. Fedorova I, Salem N, Jr. Omega-3 fatty acids and rodent behavior. Prostaglandins Leukot Essent Fatty Acids. 2006;75(4-5):271-289. (PubMed)
44. Harris WS, Von Schacky C. The omega-3 index: a new risk factor for death from coronary heart disease? Prev Med. 2004;39(1):212-220. (PubMed)
45. Metcalf RG, James MJ, Gibson RA, et al. Effects of fish-oil supplementation on myocardial fatty acids in humans. Am J Clin Nutr. 2007;85(5):1222-1228. (PubMed)
46. Owen AJ, Peter-Przyborowska BA, Hoy AJ, McLennan PL. Dietary fish oil dose- and time-response effects on cardiac phospholipid fatty acid composition. Lipids. 2004;39(10):955-961. (PubMed)
47. von Schacky C. Omega-3 index and cardiovascular health. Nutrients. 2014;6(2):799-814. (PubMed)
48. Harris WS. The omega-3 index as a risk factor for coronary heart disease. Am J Clin Nutr. 2008;87(6):1997S-2002S. (PubMed)
49. Flock MR, Skulas-Ray AC, Harris WS, Etherton TD, Fleming JA, Kris-Etherton PM. Determinants of erythrocyte omega-3 fatty acid content in response to fish oil supplementation: a dose-response randomized controlled trial. J Am Heart Assoc. 2013;2(6):e000513. (PubMed)
50. Harris WS, Pottala JV, Varvel SA, Borowski JJ, Ward JN, McConnell JP. Erythrocyte omega-3 fatty acids increase and linoleic acid decreases with age: observations from 160,000 patients. Prostaglandins Leukot Essent Fatty Acids. 2013;88(4):257-263. (PubMed)
51. Olsen SF, Sorensen JD, Secher NJ, et al. Randomised controlled trial of effect of fish-oil supplementation on pregnancy duration. Lancet. 1992;339(8800):1003-1007. (PubMed)
52. Onwude JL, Lilford RJ, Hjartardottir H, Staines A, Tuffnell D. A randomised double blind placebo controlled trial of fish oil in high risk pregnancy. Br J Obstet Gynaecol. 1995;102(2):95-100. (PubMed)
53. Smuts CM, Huang M, Mundy D, Plasse T, Major S, Carlson SE. A randomized trial of docosahexaenoic acid supplementation during the third trimester of pregnancy. Obstet Gynecol. 2003;101(3):469-479. (PubMed)
54. Zhou SJ, Yelland L, McPhee AJ, Quinlivan J, Gibson RA, Makrides M. Fish-oil supplementation in pregnancy does not reduce the risk of gestational diabetes or preeclampsia. Am J Clin Nutr. 2012;95(6):1378-1384. (PubMed)
55. Szajewska H, Horvath A, Koletzko B. Effect of n-3 long-chain polyunsaturated fatty acid supplementation of women with low-risk pregnancies on pregnancy outcomes and growth measures at birth: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2006;83(6):1337-1344. (PubMed)
56. Horvath A, Koletzko B, Szajewska H. Effect of supplementation of women in high-risk pregnancies with long-chain polyunsaturated fatty acids on pregnancy outcomes and growth measures at birth: a meta-analysis of randomized controlled trials. Br J Nutr. 2007;98(2):253-259. (PubMed)
57. Makrides M, Gibson RA, McPhee AJ, Yelland L, Quinlivan J, Ryan P. Effect of DHA supplementation during pregnancy on maternal depression and neurodevelopment of young children: a randomized controlled trial. JAMA. 2010;304(15):1675-1683. (PubMed)
58. Kar S, Wong M, Rogozinska E, Thangaratinam S. Effects of omega-3 fatty acids in prevention of early preterm delivery: a systematic review and meta-analysis of randomized studies. Eur J Obstet Gynecol Reprod Biol. 2016;198:40-46. (PubMed)
59. Carlson SE, Gajewski BJ, Alhayek S, Colombo J, Kerling EH, Gustafson KM. Dose-response relationship between docosahexaenoic acid (DHA) intake and lower rates of early preterm birth, low birth weight and very low birth weight. Prostaglandins Leukot Essent Fatty Acids. 2018;138:1-5. (PubMed)
60. Saccone G, Berghella V, Maruotti GM, Sarno L, Martinelli P. Omega-3 supplementation during pregnancy to prevent recurrent intrauterine growth restriction: systematic review and meta-analysis of randomized controlled trials. Ultrasound Obstet Gynecol. 2015;46(6):659-664. (PubMed)
61. Saccone G, Berghella V. Omega-3 supplementation to prevent recurrent preterm birth: a systematic review and metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2015;213(2):135-140. (PubMed)
62. Gould JF, Smithers LG, Makrides M. The effect of maternal omega-3 (n-3) LCPUFA supplementation during pregnancy on early childhood cognitive and visual development: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2013;97(3):531-544. (PubMed)
63. Gould JF, Treyvaud K, Yelland LN, et al. Does n-3 LCPUFA supplementation during pregnancy increase the IQ of children at school age? Follow-up of a randomised controlled trial. BMJ Open. 2016;6(5):e011465. (PubMed)
64. Muhlhausler BS, Yelland LN, McDermott R, et al. DHA supplementation during pregnancy does not reduce BMI or body fat mass in children: follow-up of the DHA to Optimize Mother Infant Outcome randomized controlled trial. Am J Clin Nutr. 2016;103(6):1489-1496. (PubMed)
65. Wood K, Mantzioris E, Lingwood B, et al. The effect of maternal DHA supplementation on body fat mass in children at 7 years: follow-up of the DOMInO randomized controlled trial. Prostaglandins Leukot Essent Fatty Acids. 2018;139:49-54. (PubMed)
66. Vahdaninia M, Mackenzie H, Dean T, Helps S. The effectiveness of omega-3 polyunsaturated fatty acid interventions during pregnancy on obesity measures in the offspring: an up-to-date systematic review and meta-analysis. Eur J Nutr. 2018; doi: 10.1007/s00394-018-1824-9. [Epub ahead of print]. (PubMed)
67. Lin J, Zhang Y, Zhu X, Wang D, Dai J. Effects of supplementation with omega-3 fatty acids during pregnancy on asthma or wheeze of children: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2018:1-10. (PubMed)
68. Vahdaninia M, Mackenzie H, Dean T, Helps S. Omega-3 LCPUFA supplementation during pregnancy and risk of allergic outcomes or sensitization in offspring: A systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2019;122(3):302-313.e302. (PubMed)
69. Delgado-Noguera MF, Calvache JA, Bonfill Cosp X, Kotanidou EP, Galli-Tsinopoulou A. Supplementation with long chain polyunsaturated fatty acids (LCPUFA) to breastfeeding mothers for improving child growth and development. Cochrane Database Syst Rev. 2015(7):Cd007901. (PubMed)
70. Guesnet P, Alessandri JM. Docosahexaenoic acid (DHA) and the developing central nervous system (CNS) - Implications for dietary recommendations. Biochimie. 2011;93(1):7-12. (PubMed)
71. Gibson RA, Kneebone GM. Fatty acid composition of human colostrum and mature breast milk. Am J Clin Nutr. 1981;34(2):252-257. (PubMed)
72. Larque E, Demmelmair H, Koletzko B. Perinatal supply and metabolism of long-chain polyunsaturated fatty acids: importance for the early development of the nervous system. Ann N Y Acad Sci. 2002;967:299-310. (PubMed)
73. Qawasmi A, Landeros-Weisenberger A, Leckman JF, Bloch MH. Meta-analysis of long-chain polyunsaturated fatty acid supplementation of formula and infant cognition. Pediatrics. 2012;129(6):1141-1149. (PubMed)
74. Qawasmi A, Landeros-Weisenberger A, Bloch MH. Meta-analysis of LCPUFA supplementation of infant formula and visual acuity. Pediatrics. 2013;131(1):e262-272. (PubMed)
75. Makrides M, Gibson RA, McPhee AJ, et al. Neurodevelopmental outcomes of preterm infants fed high-dose docosahexaenoic acid: a randomized controlled trial. JAMA. 2009;301(2):175-182. (PubMed)
76. Collins CT, Gibson RA, Anderson PJ, et al. Neurodevelopmental outcomes at 7 years' corrected age in preterm infants who were fed high-dose docosahexaenoic acid to term equivalent: a follow-up of a randomised controlled trial. BMJ Open. 2015;5(3):e007314. (PubMed)
77. Moon K, Rao SC, Schulzke SM, Patole SK, Simmer K. Longchain polyunsaturated fatty acid supplementation in preterm infants. Cochrane Database Syst Rev. 2016;12:Cd000375. (PubMed)
78. US Department of Agriculture. Agricultural Research Service. Nutrient intakes from food: mean amounts consumed per individual, by gender and age. Available at: www.ars.usda.gov/ba/bhnrc/fsrg. Accessed 4/25/14.
79. Farvid MS, Ding M, Pan A, et al. Dietary linoleic acid and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Circulation. 2014;130(18):1568-1578. (PubMed)
80. Marklund M, Wu JHY, Imamura F, et al. Biomarkers of dietary omega-6 fatty acids and incident cardiovascular disease and mortality: an individual-level pooled analysis of 30 cohort studies. Circulation. 2019; 139(21):2422-2436. (PubMed)
81. UK Medical Research Council. Controlled trial of soya-bean oil in myocardial infarction. Lancet. 1968;2(7570):693-699. (PubMed)
82. Dayton S, Pearce ML, Hashimoto S, Dixon WJ, Tomiyasu U. A controlled clinical trial of a diet high in unsaturated fat in preventing complications of atherosclerosis. Circulation. 1969;40(1s2):II-1-II-63.
83. Leren P. The Oslo diet-heart study. Eleven-year report. Circulation. 1970;42(5):935-942. (PubMed)
84. Miettinen M, Turpeinen O, Karvonen MJ, Pekkarinen M, Paavilainen E, Elosuo R. Dietary prevention of coronary heart disease in women: the Finnish mental hospital study. Int J Epidemiol. 1983;12(1):17-25. (PubMed)
85. Turpeinen O, Karvonen MJ, Pekkarinen M, Miettinen M, Elosuo R, Paavilainen E. Dietary prevention of coronary heart disease: the Finnish Mental Hospital Study. Int J Epidemiol. 1979;8(2):99-118. (PubMed)
86. Sacks FM, Lichtenstein AH, Wu JHY, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136(3):e1-e23. (PubMed)
87. Hooper L, Al-Khudairy L, Abdelhamid AS, et al. Omega-6 fats for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018;11:Cd011094. (PubMed)
88. Hamley S. The effect of replacing saturated fat with mostly n-6 polyunsaturated fat on coronary heart disease: a meta-analysis of randomised controlled trials. Nutr J. 2017;16(1):30. (PubMed)
89. Mensink RP, World Health Organization. Effects of saturated fatty acids on serum lipids and lipoproteins: a systematic review and regression analysis. 2016.
90. Mensink RP, Katan MB. Effect of dietary fatty acids on serum lipids and lipoproteins. A meta-analysis of 27 trials. Arterioscler Thromb. 1992;12(8):911-919. (PubMed)
91. Fernandez ML, West KL. Mechanisms by which dietary fatty acids modulate plasma lipids. J Nutr. 2005;135(9):2075-2078. (PubMed)
92. Ramsden CE, Zamora D, Leelarthaepin B, et al. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ. 2013;346:e8707. (PubMed)
93. Del Gobbo LC, Imamura F, Aslibekyan S, et al. Omega-3 polyunsaturated fatty Acid biomarkers and coronary heart disease: pooling project of 19 cohort studies. JAMA Intern Med. 2016;176(8):1155-1166. (PubMed)
94. Wei J, Hou R, Xi Y, et al. The association and dose-response relationship between dietary intake of alpha-linolenic acid and risk of CHD: a systematic review and meta-analysis of cohort studies. Br J Nutr. 2018;119(1):83-89. (PubMed)
95. Rimm EB, Appel LJ, Chiuve SE, et al. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: a science advisory from the American Heart Association. Circulation. 2018;138(1):e35-e47. (PubMed)
96. Bechthold A, Boeing H, Schwedhelm C, et al. Food groups and risk of coronary heart disease, stroke and heart failure: A systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr. 2017:1-20. (PubMed)
97. Zhao W, Tang H, Yang X, et al. Fish consumption and stroke risk: a meta-analysis of prospective cohort studies. J Stroke Cerebrovasc Dis. 2019;28(3):604-611. (PubMed)
98. Jayedi A, Zargar MS, Shab-Bidar S. Fish consumption and risk of myocardial infarction: a systematic review and dose-response meta-analysis suggests a regional difference. Nutr Res. 2019;62:1-12. (PubMed)
99. Zhao LG, Sun JW, Yang Y, Ma X, Wang YY, Xiang YB. Fish consumption and all-cause mortality: a meta-analysis of cohort studies. Eur J Clin Nutr. 2016;70(2):155-161. (PubMed)
100. Jayedi A, Shab-Bidar S, Eimeri S, Djafarian K. Fish consumption and risk of all-cause and cardiovascular mortality: a dose-response meta-analysis of prospective observational studies. Public Health Nutr. 2018;21(7):1297-1306. (PubMed)
101. Chowdhury R, Stevens S, Gorman D, et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta-analysis. BMJ. 2012;345:e6698. (PubMed)
102. Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation. 2011;123(24):2870-2891. (PubMed)
103. Abdelhamid AS, Brown TJ, Brainard JS, et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018;11:Cd003177. (PubMed)
104. Siscovick DS, Barringer TA, Fretts AM, et al. Omega-3 polyunsaturated fatty acid (fish oil) supplementation and the prevention of clinical cardiovascular disease: a science advisory from the American Heart Association. Circulation. 2017;135(15):e867-e884. (PubMed)
105. Di Angelantonio E, Sarwar N, Perry P, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302(18):1993-2000. (PubMed)
106. Balk EM, Lichtenstein AH, Chung M, Kupelnick B, Chew P, Lau J. Effects of omega-3 fatty acids on serum markers of cardiovascular disease risk: a systematic review. Atherosclerosis. 2006;189(1):19-30. (PubMed)
107. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation. 2002;106(21):2747-2757. (PubMed)
108. Leaf A, Xiao YF, Kang JX, Billman GE. Prevention of sudden cardiac death by n-3 polyunsaturated fatty acids. Pharmacol Ther. 2003;98(3):355-377. (PubMed)
109. Mozaffarian D, Wu JH. Omega-3 fatty acids and cardiovascular disease: effects on risk factors, molecular pathways, and clinical events. J Am Col Cardiol. 2011;58(20):2047-2067. (PubMed)
110. Howard BV. Lipoprotein metabolism in diabetes mellitus. J Lipid Res. 1987;28(6):613-628. (PubMed)
111. Khavandi M, Duarte F, Ginsberg HN, Reyes-Soffer G. Treatment of dyslipidemias to prevent cardiovascular disease in patients with type 2 diabetes. Curr Cardiol Rep. 2017;19(1):7. (PubMed)
112. Scicali R, Di Pino A, Ferrara V, et al. New treatment options for lipid-lowering therapy in subjects with type 2 diabetes. Acta Diabetol. 2018;55(3):209-218. (PubMed)
113. Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560-2572. (PubMed)
114. Zheng T, Zhao J, Wang Y, et al. The limited effect of omega-3 polyunsaturated fatty acids on cardiovascular risk in patients with impaired glucose metabolism: a meta-analysis. Clin Biochem. 2014;47(6):369-377. (PubMed)
115. Kromhout D, Giltay EJ, Geleijnse JM. n-3 fatty acids and cardiovascular events after myocardial infarction. New Engl J Med. 2010;363(21):2015-2026. (PubMed)
116. Bosch J, Gerstein HC, Dagenais GR, et al. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. New Engl J Med. 2012;367(4):309-318. (PubMed)
117. O'Mahoney LL, Matu J, Price OJ, et al. Omega-3 polyunsaturated fatty acids favourably modulate cardiometabolic biomarkers in type 2 diabetes: a meta-analysis and meta-regression of randomized controlled trials. Cardiovasc Diabetol. 2018;17(1):98. (PubMed)
118. Fox CS, Golden SH, Anderson C, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care. 2015;38(9):1777-1803. (PubMed)
119. American Diabetes Association. Management of diabetes in pregnancy: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S165-s172. (PubMed)
120. Samimi M, Jamilian M, Asemi Z, Esmaillzadeh A. Effects of omega-3 fatty acid supplementation on insulin metabolism and lipid profiles in gestational diabetes: Randomized, double-blind, placebo-controlled trial. Clin Nutr. 2015;34(3):388-393. (PubMed)
121. Taghizadeh M, Jamilian M, Mazloomi M, Sanami M, Asemi Z. A randomized-controlled clinical trial investigating the effect of omega-3 fatty acids and vitamin E co-supplementation on markers of insulin metabolism and lipid profiles in gestational diabetes. J Clin Lipidol. 2016;10(2):386-393. (PubMed)
122. Jamilian M, Samimi M, Ebrahimi FA, et al. The effects of vitamin D and omega-3 fatty acid co-supplementation on glycemic control and lipid concentrations in patients with gestational diabetes. J Clin Lipidol. 2017;11(2):459-468. (PubMed)
123. Wanders AJ, Blom WAM, Zock PL, Geleijnse JM, Brouwer IA, Alssema M. Plant-derived polyunsaturated fatty acids and markers of glucose metabolism and insulin resistance: a meta-analysis of randomized controlled feeding trials. BMJ Open Diabetes Res Care. 2019;7(1):e000585. (PubMed)
124. Wu JHY, Marklund M, Imamura F, et al. Omega-6 fatty acid biomarkers and incident type 2 diabetes: pooled analysis of individual-level data for 39 740 adults from 20 prospective cohort studies. Lancet Diabetes Endocrinol. 2017;5(12):965-974. (PubMed)
125. Hodson L, Skeaff CM, Fielding BA. Fatty acid composition of adipose tissue and blood in humans and its use as a biomarker of dietary intake. Prog Lipid Res. 2008;47(5):348-380. (PubMed)
126. Jang H, Park K. Omega-3 and omega-6 polyunsaturated fatty acids and metabolic syndrome: A systematic review and meta-analysis. Clin Nutr. 2019; doi: 10.1016/j.clnu.2019.03.032. [Epub ahead of print]. (PubMed)
127. US Centers for Disease Control and Prevention (CDC). Alzheimer's Disease. October 1, 2018. Available at: https://www.cdc.gov/aging/aginginfo/alzheimers.htm. Accessed 4/30/19.
128. Maccioni RB, Munoz JP, Barbeito L. The molecular bases of Alzheimer's disease and other neurodegenerative disorders. Arch Med Res. 2001;32(5):367-381. (PubMed)
129. Samieri C, Morris MC, Bennett DA, et al. Fish intake, genetic predisposition to Alzheimer disease, and decline in global cognition and memory in 5 cohorts of older persons. Am J Epidemiol. 2018;187(5):933-940. (PubMed)
130. Huang TL, Zandi PP, Tucker KL, et al. Benefits of fatty fish on dementia risk are stronger for those without APOE epsilon4. Neurology. 2005;65(9):1409-1414. (PubMed)
131. Whalley LJ, Deary IJ, Starr JM, et al. n-3 Fatty acid erythrocyte membrane content, APOE varepsilon4, and cognitive variation: an observational follow-up study in late adulthood. Am J Clin Nutr. 2008;87(2):449-454. (PubMed)
132. Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science. 1993;261(5123):921-923. (PubMed)
133. Plourde M, Vohl MC, Vandal M, Couture P, Lemieux S, Cunnane SC. Plasma n-3 fatty acid response to an n-3 fatty acid supplement is modulated by apoE epsilon4 but not by the common PPAR-alpha L162V polymorphism in men. Br J Nutr. 2009;102(8):1121-1124. (PubMed)
134. Chouinard-Watkins R, Rioux-Perreault C, Fortier M, et al. Disturbance in uniformly 13C-labelled DHA metabolism in elderly human subjects carrying the apoE epsilon4 allele. Br J Nutr. 2013;110(10):1751-1759. (PubMed)
135. Zhang Y, Chen J, Qiu J, Li Y, Wang J, Jiao J. Intakes of fish and polyunsaturated fatty acids and mild-to-severe cognitive impairment risks: a dose-response meta-analysis of 21 cohort studies. Am J Clin Nutr. 2016;103(2):330-340. (PubMed)
136. D'Ascoli TA, Mursu J, Voutilainen S, Kauhanen J, Tuomainen TP, Virtanen JK. Association between serum long-chain omega-3 polyunsaturated fatty acids and cognitive performance in elderly men and women: The Kuopio Ischaemic Heart Disease Risk Factor Study. Eur J Clin Nutr. 2016;70(8):970-975. (PubMed)
137. van der Lee SJ, Teunissen CE, Pool R, et al. Circulating metabolites and general cognitive ability and dementia: Evidence from 11 cohort studies. Alzheimers Dement. 2018;14(6):707-722. (PubMed)
138. Fotuhi M, Mohassel P, Yaffe K. Fish consumption, long-chain omega-3 fatty acids and risk of cognitive decline or Alzheimer disease: a complex association. Nat Clin Pract Neurol. 2009;5(3):140-152. (PubMed)
139. Sydenham E, Dangour AD, Lim WS. Omega 3 fatty acid for the prevention of cognitive decline and dementia. Cochrane Database Syst Rev. 2012(6):Cd005379. (PubMed)
140. Rangel-Huerta OD, Gil A. Effect of omega-3 fatty acids on cognition: an updated systematic review of randomized clinical trials. Nutr Rev. 2018;76(1):1-20. (PubMed)
141. Jackson PA, Forster JS, Bell JG, Dick JR, Younger I, Kennedy DO. DHA supplementation alone or in combination with other nutrients does not modulate cerebral hemodynamics or cognitive function in healthy older adults. Nutrients. 2016;8(2):86. (PubMed)
142. Kobe T, Witte AV, Schnelle A, et al. Combined omega-3 fatty acids, aerobic exercise and cognitive stimulation prevents decline in gray matter volume of the frontal, parietal and cingulate cortex in patients with mild cognitive impairment. Neuroimage. 2016;131:226-238. (PubMed)
143. Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123(20):2292-2333. (PubMed)
144. Benes LB, Bassi NS, Davidson MH. Omega-3 carboxylic acids monotherapy and combination with statins in the management of dyslipidemia. Vasc Health Risk Manag. 2016;12:481-490. (PubMed)
145. Kastelein JJ, Maki KC, Susekov A, et al. Omega-3 free fatty acids for the treatment of severe hypertriglyceridemia: the EpanoVa fOr Lowering Very high triglyceridEs (EVOLVE) trial. J Clin Lipidol. 2014;8(1):94-106. (PubMed)
146. Maki KC, Orloff DG, Nicholls SJ, et al. A highly bioavailable omega-3 free fatty acid formulation improves the cardiovascular risk profile in high-risk, statin-treated patients with residual hypertriglyceridemia (the ESPRIT trial). Clin Ther. 2013;35(9):1400-1411.e1401-1403. (PubMed)
147. Nicholls SJ, Brandrup-Wognsen G, Palmer M, Barter PJ. Meta-analysis of comparative efficacy of increasing dose of atorvastatin versus rosuvastatin versus simvastatin on lowering levels of atherogenic lipids (from VOYAGER). Am J Cardiol. 2010;105(1):69-76. (PubMed)
148. Ballantyne CM, Bays HE, Kastelein JJ, et al. Efficacy and safety of eicosapentaenoic acid ethyl ester (AMR101) therapy in statin-treated patients with persistent high triglycerides (from the ANCHOR study). Am J Cardiol. 2012;110(7):984-992. (PubMed)
149. Bays HE, McKenney J, Maki KC, Doyle RT, Carter RN, Stein E. Effects of prescription omega-3-acid ethyl esters on non--high-density lipoprotein cholesterol when coadministered with escalating doses of atorvastatin. Mayo Clin Proc. 2010;85(2):122-128. (PubMed)
150. Davidson MH, Stein EA, Bays HE, et al. Efficacy and tolerability of adding prescription omega-3 fatty acids 4 g/d to simvastatin 40 mg/d in hypertriglyceridemic patients: an 8-week, randomized, double-blind, placebo-controlled study. Clin Ther. 2007;29(7):1354-1367. (PubMed)
151. ClinicalTrials.gov. Outcomes study to assess statin residual risk reduction with Epanova in high CV risk patients with hypertriglyceridemia (STRENGTH). Available at: https://clinicaltrials.gov/ct2/show/NCT02104817. Accessed 5/24/19.
152. Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10(11):656-665. (PubMed)
153. Spooner MH, Jump DB. Omega-3 fatty acids and nonalcoholic fatty liver disease in adults and children: where do we stand? Curr Opin Clin Nutr Metab Care. 2019;22(2):103-110. (PubMed)
154. Arendt BM, Comelli EM, Ma DW, et al. Altered hepatic gene expression in nonalcoholic fatty liver disease is associated with lower hepatic n-3 and n-6 polyunsaturated fatty acids. Hepatology. 2015;61(5):1565-1578. (PubMed)
155. Yan JH, Guan BJ, Gao HY, Peng XE. Omega-3 polyunsaturated fatty acid supplementation and non-alcoholic fatty liver disease: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2018;97(37):e12271. (PubMed)
156. Gioxari A, Kaliora AC, Marantidou F, Panagiotakos DP. Intake of omega-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: A systematic review and meta-analysis. Nutrition. 2018;45:114-124.e114. (PubMed)
157. Senftleber NK, Nielsen SM, Andersen JR, et al. Marine oil supplements for arthritis pain: a systematic review and meta-analysis of randomized trials. Nutrients. 2017;9(1). (PubMed)
158. Abdulrazaq M, Innes JK, Calder PC. Effect of omega-3 polyunsaturated fatty acids on arthritic pain: A systematic review. Nutrition. 2017;39-40:57-66. (PubMed)
159. Lau CS, Morley KD, Belch JJ. Effects of fish oil supplementation on non-steroidal anti-inflammatory drug requirement in patients with mild rheumatoid arthritis--a double-blind placebo controlled study. Br J Rheumatol. 1993;32(11):982-989. (PubMed)
160. Skoldstam L, Borjesson O, Kjallman A, Seiving B, Akesson B. Effect of six months of fish oil supplementation in stable rheumatoid arthritis. A double-blind, controlled study. Scand J Rheumatol. 992;21(4):178-185. (PubMed)
161. Swan K, Allen PJ. Omega-3 fatty acid for the treatment and remission of Crohn's disease. J Complement Integr Med. 2013;10. (PubMed)
162. Feagan BG, Sandborn WJ, Mittmann U, et al. Omega-3 free fatty acids for the maintenance of remission in Crohn disease: the EPIC Randomized Controlled Trials. JAMA. 2008;299(14):1690-1697. (PubMed)
163. Cabre E, Manosa M, Gassull MA. Omega-3 fatty acids and inflammatory bowel diseases - a systematic review. Br J Nutr. 2012;107 Suppl 2:S240-252. (PubMed)
164. Lev-Tzion R, Griffiths AM, Leder O, Turner D. Omega 3 fatty acids (fish oil) for maintenance of remission in Crohn's disease. Cochrane Database Syst Rev. 2014(2):Cd006320. (PubMed)
165. Turner D, Shah PS, Steinhart AH, Zlotkin S, Griffiths AM. Maintenance of remission in inflammatory bowel disease using omega-3 fatty acids (fish oil): a systematic review and meta-analyses. Inflamm Bowel Dis. 2011;17(1):336-345. (PubMed)
166. Hodge L, Salome CM, Hughes JM, et al. Effect of dietary intake of omega-3 and omega-6 fatty acids on severity of asthma in children. Eur Respir J. 1998;11(2):361-365. (PubMed)
167. Okamoto M, Mitsunobu F, Ashida K, et al. Effects of dietary supplementation with n-3 fatty acids compared with n-6 fatty acids on bronchial asthma. Intern Med. 2000;39(2):107-111. (PubMed)
168. Wong KW. Clinical efficacy of n-3 fatty acid supplementation in patients with asthma. J Am Diet Assoc. 2005;105(1):98-105. (PubMed)
169. Schachter HM, Reisman J, Tran K, et al. Health effects of omega-3 fatty acids on asthma. Evid Rep Technol Assess (Summ). 2004(91):1-7. (PubMed)
170. Woods RK, Thien FC, Abramson MJ. Dietary marine fatty acids (fish oil) for asthma in adults and children. Cochrane Database Syst Rev. 2002(3):CD001283. (PubMed)
171. Reisman J, Schachter HM, Dales RE, et al. Treating asthma with omega-3 fatty acids: where is the evidence? A systematic review. BMC Complement Altern Med. 2006;6:26. (PubMed)
172. Donadio JV, Grande JP. IgA nephropathy. N Engl J Med. 2002;347(10):738-748. (PubMed)
173. Liu LL, Wang LN. Omega-3 fatty acids therapy for IgA nephropathy: a meta-analysis of randomized controlled trials. Clin Nephrol. 2012;77(2):119-125. (PubMed)
174. Hirahashi J. Omega-3 polyunsaturated fatty acids for the treatment of IgA nephropathy. J Clin Med. 2017;6(7). (PubMed)
175. Brigandi SA, Shao H, Qian SY, Shen Y, Wu BL, Kang JX. Autistic children exhibit decreased levels of essential fatty acids in red blood cells. Int J Mol Sci. 2015;16(5):10061-10076. (PubMed)
176. Mazahery H, Stonehouse W, Delshad M, et al. Relationship between long chain n-3 polyunsaturated fatty acids and autism spectrum disorder: systematic review and meta-analysis of case-control and randomised controlled trials. Nutrients. 2017;9(2). (PubMed)
177. Yui K, Koshiba M, Nakamura S, Kobayashim Y, Ohnishi M. Efficacy of adding large doses of arachidonic acid to docosahexaenoic acid against restricted repetitive behaviors in individuals with autism spectrum disorders: a placebo-controlled trial. J Addict Res Ther. 2011;S4(006).
178. Amminger GP, Berger GE, Schafer MR, Klier C, Friedrich MH, Feucht M. Omega-3 fatty acids supplementation in children with autism: a double-blind randomized, placebo-controlled pilot study. Biol Psychiatry. 2007;61(4):551-553. (PubMed)
179. Bent S, Bertoglio K, Ashwood P, Bostrom A, Hendren RL. A pilot randomized controlled trial of omega-3 fatty acids for autism spectrum disorder. J Autism Dev Disord. 2011;41(5):545-554. (PubMed)
180. Bent S, Hendren RL, Zandi T, et al. Internet-based, randomized, controlled trial of omega-3 fatty acids for hyperactivity in autism. J Am Acad Child Adolesc Psychiatry. 2014;53(6):658-666. (PubMed)
181. Mankad D, Dupuis A, Smile S, et al. A randomized, placebo controlled trial of omega-3 fatty acids in the treatment of young children with autism. Mol Autism. 2015;6:18. (PubMed)
182. Voigt RG, Mellon MW, Katusic SK, et al. Dietary docosahexaenoic acid supplementation in children with autism. J Pediatr Gastroenterol Nutr. 2014;58(6):715-722. (PubMed)
183. Cheng YS, Tseng PT, Chen YW, et al. Supplementation of omega 3 fatty acids may improve hyperactivity, lethargy, and stereotypy in children with autism spectrum disorders: a meta-analysis of randomized controlled trials. Neuropsychiatr Dis Treat. 2017;13:2531-2543. (PubMed)
184. Horvath A, Lukasik J, Szajewska H. Omega-3 fatty acid supplementation does not affect autism spectrum disorder in children: a systematic review and meta-analysis. J Nutr. 2017;147(3):367-376. (PubMed)
185. Hibbeln JR. Fish consumption and major depression. Lancet. 1998;351(9110):1213. (PubMed)
186. Noaghiul S, Hibbeln JR. Cross-national comparisons of seafood consumption and rates of bipolar disorders. Am J Psychiatry. 2003;160(12):2222-2227. (PubMed)
187. Maes M, Christophe A, Delanghe J, Altamura C, Neels H, Meltzer HY. Lowered omega3 polyunsaturated fatty acids in serum phospholipids and cholesteryl esters of depressed patients. Psychiatry Res. 1999;85(3):275-291. (PubMed)
188. Peet M, Murphy B, Shay J, Horrobin D. Depletion of omega-3 fatty acid levels in red blood cell membranes of depressive patients. Biol Psychiatry. 1998;43(5):315-319. (PubMed)
189. Tiemeier H, van Tuijl HR, Hofman A, Kiliaan AJ, Breteler MM. Plasma fatty acid composition and depression are associated in the elderly: the Rotterdam Study. Am J Clin Nutr. 2003;78(1):40-46. (PubMed)
190. Mamalakis G, Tornaritis M, Kafatos A. Depression and adipose essential polyunsaturated fatty acids. Prostaglandins Leukot Essent Fatty Acids. 2002;67(5):311-318. (PubMed)
191. Locke CA, Stoll AL. Omega-3 fatty acids in major depression. World Rev Nutr Diet. 2001;89:173-185. (PubMed)
192. Ortega RM, Rodriguez-Rodriguez E, Lopez-Sobaler AM. Effects of omega 3 fatty acids supplementation in behavior and non-neurodegenerative neuropsychiatric disorders. Br J Nutr. 2012;107 Suppl 2:S261-270. (PubMed)
193. Prior PL, Galduroz JC. (N-3) Fatty acids: molecular role and clinical uses in psychiatric disorders. Adv Nutr. 2012;3(3):257-265. (PubMed)
194. Grosso G, Pajak A, Marventano S, et al. Role of omega-3 fatty acids in the treatment of depressive disorders: a comprehensive meta-analysis of randomized clinical trials. PLoS One. 2014;9(5):e96905. (PubMed)
195. Appleton KM, Sallis HM, Perry R, Ness AR, Churchill R. Omega-3 fatty acids for major depressive disorder in adults: an abridged Cochrane review. BMJ Open. 2016;6(3):e010172. (PubMed)
196. McNamara RK, Welge JA. Meta-analysis of erythrocyte polyunsaturated fatty acid biostatus in bipolar disorder. Bipolar Disord. 2016;18(3):300-306. (PubMed)
197. Shakeri J, Khanegi M, Golshani S, et al. Effects of omega-3 supplement in the treatment of patients with bipolar I disorder. Int J Prev Med. 2016;7:77. (PubMed)
198. Hoen WP, Lijmer JG, Duran M, Wanders RJ, van Beveren NJ, de Haan L. Red blood cell polyunsaturated fatty acids measured in red blood cells and schizophrenia: a meta-analysis. Psychiatry Res. 2013;207(1-2):1-12. (PubMed)
199. Akter K, Gallo DA, Martin SA, et al. A review of the possible role of the essential fatty acids and fish oils in the aetiology, prevention or pharmacotherapy of schizophrenia. J Clin Pharm Ther. 2012;37(2):132-139. (PubMed)
200. Robinson DG, Gallego JA, John M, et al. A potential role for adjunctive omega-3 polyunsaturated fatty acids for depression and anxiety symptoms in recent onset psychosis: Results from a 16week randomized placebo-controlled trial for participants concurrently treated with risperidone. Schizophr Res. 2019;204:295-303. (PubMed)
201. Burckhardt M, Herke M, Wustmann T, Watzke S, Langer G, Fink A. Omega-3 fatty acids for the treatment of dementia. Cochrane Database Syst Rev. 2016;4:Cd009002. (PubMed)
202. Freund-Levi Y, Eriksdotter-Jonhagen M, Cederholm T, et al. Omega-3 fatty acid treatment in 174 patients with mild to moderate Alzheimer disease: OmegAD study: a randomized double-blind trial. Arch Neurol. 2006;63(10):1402-1408. (PubMed)
203. Shinto L, Quinn J, Montine T, et al. A randomized placebo-controlled pilot trial of omega-3 fatty acids and alpha lipoic acid in Alzheimer's disease. J Alzheimers Dis. 2014;38(1):111-120. (PubMed)
204. Quinn JF, Raman R, Thomas RG, et al. Docosahexaenoic acid supplementation and cognitive decline in Alzheimer disease: a randomized trial. JAMA. 2010;304(17):1903-1911. (PubMed)
205. US Department of Agriculture ARS. USDA National Nutrient Database for Standard Reference, Release 26. Available at: http://www.ars.usda.gov/ba/bhnrc/ndl. Accessed 4/25/14.
206. Hendler SS, Rorvik DM. PDR for nutritional supplements: Thomson Reuters New Jersey; 2008.
207. Ulven SM, Kirkhus B, Lamglait A, et al. Metabolic effects of krill oil are essentially similar to those of fish oil but at lower dose of EPA and DHA, in healthy volunteers. Lipids. 2011;46(1):37-46. (PubMed)
208. US Food and Drug Administration. CfFSaAN. Agency Response Letter: GRAS Notice No. GRN 000080. 2001. Available at: http://www.cfsan.fda.gov/~rdb/opa-g080.html. Accessed 11/7/08.
209. Zurier RB, Rossetti RG, Jacobson EW, et al. gamma-Linolenic acid treatment of rheumatoid arthritis. A randomized, placebo-controlled trial. Arthritis Rheum. 1996;39(11):1808-1817. (PubMed)
210. Vaddadi KS. The use of gamma-linolenic acid and linoleic acid to differentiate between temporal lobe epilepsy and schizophrenia. Prostaglandins Med. 1981;6(4):375-379. (PubMed)
211. Nordstrom DC, Honkanen VE, Nasu Y, Antila E, Friman C, Konttinen YT. Alpha-linolenic acid in the treatment of rheumatoid arthritis. A double-blind, placebo-controlled and randomized study: flaxseed vs. safflower seed. Rheumatol Int. 1995;14(6):231-234. (PubMed)
212. Alonso L, Marcos ML, Blanco JG, et al. Anaphylaxis caused by linseed (flaxseed) intake. J Allergy Clin Immunol. 1996;98(2):469-470. (PubMed)
213. Harbige LS. Fatty acids, the immune response, and autoimmunity: a question of n-6 essentiality and the balance between n-6 and n-3. Lipids. 2003;38(4):323-341. (PubMed)
214. Carlson SE, Cooke RJ, Werkman SH, Tolley EA. First year growth of preterm infants fed standard compared to marine oil n-3 supplemented formula. Lipids. 1992;27(11):901-907. (PubMed)
215. Carlson SE, Werkman SH, Tolley EA. Effect of long-chain n-3 fatty acid supplementation on visual acuity and growth of preterm infants with and without bronchopulmonary dysplasia. Am J Clin Nutr. 1996;63(5):687-697. (PubMed)
216. Schulzke SM, Patole SK, Simmer K. Long-chain polyunsaturated fatty acid supplementation in preterm infants. Cochrane Database Syst Rev. 2011(2):CD000375. (PubMed)
217. Hendler SS, Rorvik DR, eds. PDR for Nutritional Supplements. Montvale: Medical Economics Company, Inc; 2001.
218. Mozaffarian D, Rimm EB. Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA. 2006;296(15):1885-1899. (PubMed)
219. Environmental Protection Agency. Fish Advisories [Web site]. April 14, 2003. Available at: http://www.epa.gov/waterscience/fish/. Accessed 4/28/03.
220. 2015-2020 Dietary Guidelines for Americans. Available at: https://health.gov/dietaryguidelines/2015/guidelines/. Accessed 5/24/19.
221. Consumer Lab. Product Review: FIsh oil and omega-3 fatty acid supplements review (including krill, algae, calamari, green-lipped mussel oil). Available at: http://www.consumerlab.com/results/omega3.asp. Accessed 4/25/14.
222. Hilbert G, Lillemark L, Balchen S, Hojskov CS. Reduction of organochlorine contaminants from fish oil during refining. Chemosphere. 1998;37(7):1241-1252. (PubMed)
223. Bender NK, Kraynak MA, Chiquette E, Linn WD, Clark GM, Bussey HI. Effects of marine fish oils on the anticoagulation status of patients receiving chronic warfarin therapy. J Thromb Thrombolysis. 1998;5(3):257-261. (PubMed)
224. Buckley MS, Goff AD, Knapp WE. Fish oil interaction with warfarin. Ann Pharmacother. 2004;38(1):50-52. (PubMed)
225. Valk EE, Hornstra G. Relationship between vitamin E requirement and polyunsaturated fatty acid intake in man: a review. Int J Vitam Nutr Res. 2000;70(2):31-42. (PubMed)
226. Higdon JV, Liu J, Du SH, Morrow JD, Ames BN, Wander RC. Supplementation of postmenopausal women with fish oil rich in eicosapentaenoic acid and docosahexaenoic acid is not associated with greater in vivo lipid peroxidation compared with oils rich in oleate and linoleate as assessed by plasma malondialdehyde and F(2)-isoprostanes. Am J Clin Nutr. 2000;72(3):714-722. (PubMed)
227. Wander RC, Du SH, Ketchum SO, Rowe KE. alpha-Tocopherol influences in vivo indices of lipid peroxidation in postmenopausal women given fish oil. J Nutr. 1996;126(3):643-652. (PubMed)
228. Wander RC, Du SH. Oxidation of plasma proteins is not increased after supplementation with eicosapentaenoic and docosahexaenoic acids. Am J Clin Nutr. 2000;72(3):731-737. (PubMed)
229. Larque E, Gil-Sanchez A, Prieto-Sanchez MT, Koletzko B. Omega 3 fatty acids, gestation and pregnancy outcomes. Br J Nutr. 2012;107 Suppl 2:S77-84. (PubMed)
230. American Heart Association. Frequently Asked Questions About Fish. Available at: http://www.heart.org/HEARTORG/General/Frequently-Asked-Questions-About-Fish_UCM_306451_Article.jsp. Accessed 4/25/14.
231. EFSA Panel on Dietetic Products, Nutrition, and Allergies (NDA). Scientific opinion on dietary reference values for fats, including saturated fatty acids, polyunsaturated fatty acids, monounsaturated fatty acids, trans fatty acids, and cholesterol. EFSA Journal. 2010;8(3):107.
232. European Food Safety Authority. The DRV Finder. Available at: https://www.efsa.europa.eu/en/interactive-pages/drvs. Accessed 5/24/19.
233. FAO/WHO. Interim Summary of Conclusions and Dietary Recommendations on Total Fat & Fatty Acids. Joint FAO/WHO Expert Consultation on Fats and Fatty Acids in Human Nutrition. Geneva: WHO; 2008:1-14.
234. International Society for the Study of Fatty Acids and Lipids (ISSFAL). Recommendations for intake of polyunsaturated fatty acids in healthy adults. Available at: https://www.issfal.org/statement-3. Accessed 4/24/19.
Fiber
Contents
Summary
- Dietary fiber is a diverse group of compounds, including lignin and complex carbohydrates, which cannot be digested by human enzymes in the small intestine. (More information)
- Although each fiber type is chemically unique, fibers can be classified according to their solubility, viscosity, and fermentability in order to better understand their physiological effects. (More information)
- Soluble gel-forming fibers, such as psyllium and fibers found in oat products, can lower serum LDL cholesterol concentrations and normalize blood glucose and insulin responses. (More information)
- Large/coarse insoluble fibers (e.g., wheat bran) and nonfermentable, soluble gel-forming fibers (e.g., psyllium) can have a potential laxative effect. (More information)
- Large prospective cohort studies consistently report inverse associations between consumption of diets rich in fiber and risks of cardiovascular disease and type 2 diabetes mellitus. (More information)
- A review of the most recent meta-analyses of observational studies suggests that dietary fiber consumption is inversely associated with the risk of cancer of the esophagus, stomach, colon, pancreas, ovary, and breast. (More information)
- Both consumption of fiber-rich diets and supplementation with soluble gel-forming fibers could help improve glycemic control in individuals with type 1 or type 2 diabetes mellitus. (More information)
- The Adequate Intake (AI) recommendation for total daily fiber intake is 38 g/day for men and 25 g/day for women. However, the average American consumes only about 17 g/day of dietary fiber, and dietary fiber intake might be closer to 10 g/day in those following a low-carbohydrate diet. (More information)
- Some strategies for increasing dietary fiber intake include increasing fruit and nonstarchy vegetable intake, increasing intake of legumes, eating whole-grain cereal or oatmeal for breakfast, substituting whole grains for refined grains, and substituting nuts or popcorn for less healthy snacks. (More information)
Introduction
All dietary fibers are resistant to digestion in the small intestine, meaning they arrive intact in the large intestine (1). Although most fibers are carbohydrates, one important factor that determines their susceptibility to digestion by human enzymes is the conformation of the chemical bonds between sugar molecules (glycosidic bonds). Humans lack digestive enzymes capable of hydrolyzing (breaking apart) most β-glycosidic bonds, which explains why amylose, a glucose polymer with α-1,4 glycosidic bonds, is digestible by human enzymes, while cellulose, a glucose polymer with β-1,4 glycosidic bonds, is indigestible (Figure 1).
Definitions of Fiber
Although nutritional scientists and clinicians generally agree that a healthy diet should include plenty of fiber-rich foods, agreement on the actual definition of fiber has been more difficult to achieve (2-4). In the 1970s, dietary fiber was defined as remnants of plant cells that are resistant to digestion by human enzymes (5). This definition includes a component of some plant cell walls called lignin, as well as indigestible carbohydrates found in plants. However, this definition omits indigestible carbohydrates derived from animal sources (e.g., chitin) and synthetic (e.g., fructooligosaccharides, polydextrose, wheat dextrin) and carbohydrates that are inaccessible to human digestive enzymes (e.g., resistant starch) (6). These compounds share many of the characteristics of fiber present in plant foods.
Institute of Medicine: dietary, functional, and total fiber
Before establishing intake recommendations for fiber in 2001, a panel of experts convened by the Institute of Medicine (now the National Academy of Medicine) developed definitions of fiber that made a distinction between fiber that occurs naturally in plant foods (dietary fiber) and isolated or synthetic fibers that may be added to foods or used as dietary supplements (functional fiber) (4). However, these distinctions are controversial, and there are other classification systems for dietary fiber (see Other classification systems below).
Dietary fiber
- Lignin: Lignin is not a carbohydrate; rather, it is a polyphenolic compound with a complex three-dimensional structure that is found in the cell walls of woody plants and seeds (7).
- Cellulose: Cellulose is a glucose polymer with β-1,4 glycosidic bonds found in all plant cell walls (Figure 1) (6).
- β-Glucans: β-Glucans are glucose polymers with a mixture of β-1,4 glycosidic bonds and β-1,3 glycosidic bonds (Figure 1). Oats and barley are particularly rich in β-glucans (7).
- Hemicelluloses: Hemicelluloses are a diverse group of polysaccharides (sugar polymers) containing different types of sugar monomers, including glucose, xylose, arabinose, mannose, galactose, rhamnose, or pentose. Glucomannan is a hemicellulose containing about 60% of mannose and 40% of glucose bonded together by β-1,4 glycosidic linkages. Like cellulose, hemicelluloses are found in plant cell walls.
- Pectins: Pectins are linear polysaccharides made of 300 to 1,000 monosaccharides, primarily galacturonic acid residues linked together by α-1,4 glycosidic bonds (8). Pectins are soluble viscous fibers that are particularly abundant in berries and other fruit (4).
- Gums: Gums are viscous polysaccharides often found in seeds (4). Guar gum extracted from guar beans is a galactomannan polysaccharide composed of mannose and galactose residues. It is used in the food industry for its thickening and stabilizing properties. The viscosity of guar gum is lost when guar gum is partially hydrolyzed to derive partially hydrolyzed guar gum (PHGG).
- Inulin and oligofructose: Inulin is a mixture of fructose chains that vary in length and often terminate with a glucose molecule (9). Oligofructose is a mixture of shorter fructose chains that may terminate in glucose or fructose. Inulin and oligofructose occur naturally in plants, such as onions and Jerusalem artichokes.
- Resistant starch: Naturally occurring resistant starch is sequestered in plant cell walls and is therefore inaccessible to human digestive enzymes (4). It is fermented by bacteria in the colon. Bananas and legumes are sources of naturally occurring resistant starch. Resistant starch may also be formed by food processing or by cooling and reheating.
Functional fiber
According to the Institute of Medicine’s definition, functional fiber "consists of isolated, nondigestible carbohydrates that have beneficial physiological effects in humans" (4). Functional fibers may be nondigestible carbohydrates that have been isolated or extracted from a natural plant or animal source, or they may be manufactured or synthesized. However, designation as a functional fiber by the Institute of Medicine requires the presentation of sufficient evidence of physiological benefit in humans. Fibers identified as potential functional fibers by the Institute of Medicine include:
- Isolated or extracted forms of the dietary fibers listed above.
- Psyllium: Psyllium refers to viscous, gel-forming mucilage, which is isolated from the outer coat (husk) of psyllium seeds — known in India as ispaghula husk — from the plant Plantago ovata or blond psyllium (4).
- Chitin and chitosan: Chitin is a polysaccharide polymer extracted from the exoskeletons of crustaceans, such as crab and lobster. It is a polymer of more than 5,000 acetylated glucosamine units linked by β-1,4 glycosidic bonds. Deacetylated chitin or chitosan thus consists in unbranched chains of glucosamine (8).
- Fructooligosaccharides: Fructooligosaccharides are short, synthetic fructose chains terminating with a glucose unit. They are used as food additives (9).
- Galactooligosaccharides: Galactooligosaccharides are produced through the enzymatic conversion of lactose and are classified as prebiotics (10).
- Polydextrose and polyols: Polydextrose and polyols are synthetic carbohydrates. Polydextrose is made of glucose and sorbitol (a sugar alcohol) and may be used as bulking agent in food. Polyols are non-sugar molecules containing multiple hydroxyl groups (-OH). Polydextrose and polyols are used as sugar substitutes in food (4).
- Resistant dextrins: Resistant dextrins, also called resistant maltodextrins, are synthetic indigestible polysaccharides formed when starch is heated and treated with enzymes. They are used as food additives (4).
Total fiber
Total fiber is defined by the Institute of Medicine as "the sum of dietary fiber and functional fiber" (4).
Other classification systems
Fibers can be classified into four clinically meaningful categories according to their physiochemical properties, i.e., their solubility, viscosity, and fermentability (reviewed in 11):
Soluble, viscous/gel forming, readily fermented fibers
E.g., β-glucans from oats and barley, raw guar gum
Soluble fibers dissolve in water, while insoluble fibers do not. Viscous fibers thicken in the presence of water, forming very viscous solutions or even visco-elastic gels. Fermentable fibers are readily metabolized by the gut microbiota (i.e., bacteria that normally colonize the large intestine). Fermentation of fiber results in the formation of short-chain fatty acids (acetate, propionate, and butyrate) and gases (1). Short-chain fatty acids can be absorbed and metabolized to produce energy. Interestingly, the preferred energy source for colonocytes (epithelial cells that line the colon) is butyrate. Fermentation of fiber is estimated to contribute up to 10% of daily energy intake (12). Fibers that are fermentable and can stimulate the growth and/or activity of beneficial gut bacteria are called prebiotic fibers (13). Fibers that are soluble, viscous, and fermentable have been shown to improve glycemic control and to lower blood cholesterol concentration. However, their water-holding capacity is lost when they are fermented in the colon such that they have no laxative effect (see Biological Activities).
Soluble, viscous/gel forming, nonfermented fibers
E.g., psyllium
These fibers can dissolve in water and form viscous gels. They can improve glycemic control and lower blood cholesterol concentration. In addition, they retain their water-holding/gel-forming capacity in the large intestine since they are resistant to fermentation. As a consequence, they can exert a stool-normalizing effect, preventing constipation or softening hard stool as well as firming loose/liquid stool in diarrhea and fecal incontinence (see Biological Activities).
Soluble, nonviscous, readily fermented fibers
E.g., inulin, wheat dextrin, oligosaccharides, resistant starches
Although these fibers can dissolve in water, they cannot provide any health benefits associated with fiber viscosity. They are fully fermented and thus do not exert a laxative effect. They can nonetheless exert a prebiotic effect by influencing the composition of the gut microbiota. In vitro studies have shown inulin to selectively stimulate the proliferation of beneficial bacteria and limit the growth of potentially pathogenic bacteria ) (see Isolated fibers and supplements) (reviewed in 14). However, no health benefit is currently associated with this fiber-driven prebiotic effect.
Insoluble, poorly fermented fibers
E.g., wheat bran, cellulose, lignin
These fibers do not dissolve in water, do not trap water, and are poorly fermented. Large/coarse fiber particles can have a laxative effect. They can irritate the large intestine mucosa and trigger the secretion of mucus and water, which increases the water content of stools. Small, insoluble fiber particles (e.g., finely ground wheat bran) have no laxative effect and can actually have a constipating effect by adding only to the dry stool mass (see Improving regularity in stool elimination).
Biological Activities
Lowering serum cholesterol
Some, but not all, fibers can improve blood lipid abnormalities observed in conditions like dyslipidemia, overweight/obesity, type 2 diabetes mellitus, and metabolic syndrome. Only supplementation with highly viscous fibers (i.e., gel-forming soluble fibers), such as high molecular weight (MW) β-glucan (found in oat bran), raw guar gum, and psyllium, has been shown to decrease total and LDL-cholesterol concentrations when compared to appropriate controls (e.g., fiber-free supplement, low-fiber supplement, or supplementation with insoluble fiber) (15). A 2009 meta-analysis that combined the results of 21 randomized controlled trials in 1,717 participants with hypercholesterolemia found dose- and time-dependent reductions in total and LDL-cholesterol concentrations with psyllium supplementation (3.0-20.4 g/day for >2 weeks) (16). Additionally, results from two trials showed that, compared to statins alone, combining psyllium and statins resulted in larger reductions in LDL-cholesterol concentrations in individuals with hypercholesterolemia (17). Another more recent meta-analysis of 28 randomized controlled trials examined the cholesterol-lowering effect of psyllium fiber on LDL-cholesterol, non-HDL-cholesterol, and apolipoprotein B (apo B) (18) — non-HDL-cholesterol and apo B appear to better predict cardiovascular events than LDL-cholesterol (19). Supplementation with psyllium at a median dose of 10.2 g/day and for a median of eight weeks to participants with or without hypercholesterolemia reduced LDL-cholesterol by 0.33 mmol/L (28 trials; 1,924 participants), non-HDL-cholesterol by 0.39 mmol/L (27 trials; 1,899 participants), and apo B by 0.05 g/L (9 trials; 895 participants) (18).
Despite considerable heterogeneity across studies, the cholesterol-lowering efficacy of other highly viscous fibers, including β-glucans from oat or barley and glucomannan (a hemicellulose), was also reported in recent meta-analyses of trials conducted by one research team (20-22). The cholesterol-lowering effect of soluble fibers, such as psyllium and β-glucan, is directly linked to their high viscosity. Reduction of the gel-forming capacity of these fibers with pressure and/or heat during processing leads to the loss of their cholesterol lowering capacity (23). Accordingly, low-viscosity soluble fibers (e.g., gum arabic/acacia gum, methylcellulose, low MW β-glucan), nonviscous soluble fermentable fibers (e.g., inulin, fructooligosaccharides, wheat dextrin), and insoluble fibers (e.g., wheat bran) do not decrease serum cholesterol at physiologic levels (15).
Highly viscous fibers can trap bile that is released in the small intestine in response to a meal to assist the digestion and absorption of fatty acids. The main mechanism underlying the cholesterol-lowering effect of these fibers is thus linked to their ability to prevent the reabsorption of bile in the terminal ileum and facilitate its elimination in the stool. In order to maintain sufficient bile for digestion, hepatocytes must increase LDL-cholesterol clearance to synthesize more bile acids as cholesterol is a component of bile (15).
These findings led the FDA to approve health claims in relation to the prevention of heart disease on labels of low cholesterol/saturated fat foods containing ≥0.75 g/serving of β-glucan from whole oat or barley or ≥1.7 g/serving of psyllium (see also Cardiovascular disease) (24).
Improving glycemic control
As with cholesterol lowering, the efficacy of fiber on glycemic control is dependent on viscosity. A 2017 review of 14 randomized controlled trials showed that none of the supplemented soluble, nonviscous, fermentable fibers examined (i.e., inulin, fructooligosaccharide, galactooligosaccharide, and oligofructose) could lead to reductions in postprandial and/or fasting blood glucose concentrations (15). Supplementation with insoluble fiber also failed to improve glycemic control in subjects with elevated fasting blood glucose concentrations (25). In contrast, the capacity of dietary viscous fiber (26, 27) and isolated viscous fibers (28-31) to improve glycemic control has been demonstrated in numerous controlled clinical trials conducted over three decades (15). A 2015 review of the efficacy of psyllium showed evidence of reductions in postprandial blood glucose concentration following a single meal in people with type 2 diabetes mellitus (6 studies) as well as in nondiabetic/euglycemic subjects (11 studies) (32). Supplementation with psyllium also resulted in reductions in postprandial blood insulin concentrations in subjects without type 2 diabetes (6 studies) but not in those with type 2 diabetes (3 studies). Longer-term studies of psyllium supplementation also found reductions in mean fasting glucose (4 studies) and mean glycated hemoglobin (HbA1c; 3 studies) in subjects with type 2 diabetes. Finally, while there was no effect of long-term exposure to psyllium on fasting glucose concentration in healthy individuals with euglycemia (14 studies), the glycemic benefit of psyllium was found to increase proportionally with the increase of baseline fasting glucose concentration (reviewed in 32).
The role of soluble viscous fibers on glycemic control is related to their ability to increase chyme viscosity, thereby slowing the degradation of complex nutrients and allowing the absorption of nutrients, including glucose, along the entire small intestine rather than in the upper small intestine. Absorption of nutrients in the distal ileum has been associated with a reduction in gastric emptying and intestinal transit — through a distal to proximal feedback mechanism — which in turn reduces hunger and food intake (reviewed in 15). Nutrient delivery in the distal ileum also triggers the release of short-lived glucagon-like peptide 1 (GLP-1) into the circulation. GLP-1 improves insulin secretion by pancreatic β-cells in response to glucose absorption and is involved in the regulation of food intake at the central nervous system level (33).
Lowering blood pressure
An analysis of 2004-2014 US National Health and Nutrition Examination Survey (NHANES) data from 18,433 participants found inverse associations between either total, cereal, or vegetable fiber intake and the odds of hypertension (defined according to new 2017 American College of Cardiology/American Heart Association clinical practice guidelines; 34). A 2018 meta-analysis of 22 randomized control trials that examined the effect of isolated soluble fiber supplements or diets enriched with soluble viscous fiber in either normotensive or hypertensive participants found an overall 1.59 mm Hg reduction in systolic blood pressure and 0.39 mm Hg reduction in diastolic blood pressure (35). Further analyses showed that, among all the soluble viscous fiber under examination (β-glucan, guar gum, konjac glucomannan, pectin, and psyllium), only psyllium could reduce systolic blood pressure (mean reduction of 2.39 mm Hg) (35). It is not yet understood how soluble viscous fiber would induce a lowering of blood pressure, but this effect may be indirect and dependent on established benefits of these fiber on other cardiometabolic parameters (see the above sections).
Improving regularity in stool elimination
The benefit of fiber on the regularity with which bulky, soft, easy-to-pass stools are eliminated is best assessed by an increase in stool output and an increase in the water content of stool. There are two mechanisms that support the laxative effects of certain fiber types: (i) large/coarse insoluble fiber (e.g., wheat bran) has an irritating effect on the colonic mucosa, which stimulates the secretion of water and mucus (unlike finely ground wheat bran that has a stool-hardening/constipating effect); and (ii) the presence of soluble viscous, gel-forming fiber (e.g., psyllium) helps stool to resist dehydration in the colon (15). Therefore, only fibers that remain relatively intact during the transit throughout the length of the colon (i.e., that resists bacterial fermentation) and are thus found in the stool can have a potential laxative effect. A 2016 review of fiber interventions conducted by McRorie and Chey (36) examined the potential laxative effect of fermentable fiber; the main findings of this review are summarized in Table 1.
| Fiber | Type of Fiber | Number of Studies | Doses | Laxative Effects | Adverse Effects |
|---|---|---|---|---|---|
|
β-Glucan, guar gum, xanthan gum
|
Soluble, viscous, fermentable | 5 studies: all conducted in healthy participants; 3 studies with β-glucan and 2 studies (guar gum, xanthan gum) | 87-100 g/day (β-glucan) and 15 g/day (guar gum, xanthan gum) |
• Stool hardening effect and minimal increase in stool output (β-glucan) • No effect on stool output and stool consistency (guar gum, xanthan gum) |
Not reported
|
| Inulin | Soluble, nonviscous, fermentable | 11 studies: 3 studies in people with constipation and 8 studies in healthy people | 5-20 g/day | • No effect on colonic transit time, stool consistency, stool water content, or stool output |
Abdominal pain, bloating, flatulence, and borborygmus (1 study) |
| Polydextrose | Soluble, nonviscous, fermentable | 6 studies: all conducted in healthy participants | 8-30 g/day | • No effect on stool output, consistency, bowel movement frequency, or colonic transit time | Flatulence and borborygmus (1 study) |
| Resistant starch (incl. resistant dextrin) | Soluble, nonviscous, fermentable | 6 studies: all conducted in healthy participants | 7.5-15 g/day |
• Stool hardening effect and reduction in stool output (2 studies) • No effect on consistency, stool water content, stool output, or bowel movement frequency (4 studies) |
Not reported |
In summary, although the bulk of evidence comes primarily from studies in healthy subjects, supplementation with fermentable fibers appears unlikely to exert a laxative effect in people suffering from constipation (Table 1). In contrast, a 2016 meta-analysis of seven randomized controlled trials identified psyllium and nonprebiotics as effectively able to increase stool frequency and improve stool consistency in participants affected by chronic idiopathic constipation (see also Chronic idiopathic constipation) (37) .
Disease Prevention
Observational studies that have identified associations between high-fiber intakes and reductions in chronic disease risk have generally assessed only fiber-rich foods, rather than fiber itself, making it difficult to determine whether the observed benefits are related to fiber or other nutrients and phytochemicals commonly found in fiber-rich foods. In contrast, intervention trials often use isolated fibers to determine whether a specific fiber component has beneficial health effects.
Cardiovascular disease
Prospective cohort studies have consistently reported associations between high intakes of fiber-rich foods and low risks of coronary heart disease (CHD) and total cardiovascular disease (CVD). Three large prospective cohort studies (38-40) found that dietary fiber intakes of approximately 14 g per 1,000 kcal of energy were associated with substantial (16-33%) decreases in the risk of CHD; these results are the basis for the Institute of Medicine’s Adequate Intake (AI) recommendation for fiber (see Intake Recommendations) (4). A 2013 meta-analysis of 17 prospective cohort studies found each 7 g/day increase in total dietary fiber intake to be associated with a 9% decrease in risk of coronary or total cardiovascular events (41). The most recent meta-analysis that included 18 prospective studies, with a total of 672,408 participants, found a 7% lower risk of CHD and a 17% lower risk of CHD-related mortality with the highest versus lowest intakes of total dietary fiber (42). Subgroup analyses by type or source of dietary fiber showed evidence of inverse associations between cereal, fruit, or soluble fiber intake and the risk of CHD (42).
The US FDA has approved health claims like the following on the labels of foods containing at least 0.75 g/serving of β-glucan soluble fiber: "Diets low in saturated fat and cholesterol that include at least 3 g/day of β-glucan soluble fiber from either whole oats or barley or a combination of both may reduce the risk of coronary heart disease" (24). Similarly, the FDA has approved health claims on the labels of foods containing at least 1.7 g/serving of psyllium: "Diets low in saturated fat and cholesterol that include at least 7 g/day of soluble fiber from psyllium seed husk may reduce the risk of heart disease" (24).
While the cholesterol-lowering effect of viscous/gel-forming soluble fibers is recognized as a major contributor to the cardioprotective effects of fiber (see Lowering serum cholesterol), other mechanisms are likely to be involved. Findings from pooled analyses of prospective cohort studies found some evidence of an inverse association between the risks of CHD and total CVD and intakes of insoluble fiber (41, 42). In addition, a cross-sectional analysis of 2005-2010 National Health and Nutrition Examination Survey (NHANES) data found dietary fiber intake to be inversely associated with serum LDL-cholesterol concentration, but also with blood pressure, body mass index (BMI), and serum insulin concentration (43). Beneficial effects of fiber-rich diets or isolated fiber consumption on blood glucose and insulin responses and on blood pressure may also likely contribute to observed reductions in CHD risk (see Biological Activities).
Type 2 diabetes mellitus
A 2014 meta-analysis of prospective cohort studies (488,293 participants) found intakes of total fiber (12 studies), cereal fiber (10 studies), fruit fiber (8 studies), and insoluble fiber (3 studies) to be inversely associated with the risk of developing type 2 diabetes mellitus (44). A dose-response data analysis reported a nonlinear relationship between total fiber intake and diabetes risk, with evidence of risk reduction with total fiber intakes ≥25 g/day. A linear dose-response relationship between cereal fiber intake and diabetes risk indicated a 6% reduction in diabetes risk for each 2 g-increment in daily cereal fiber intake. There was no evidence of an inverse association between either vegetable fiber (9 studies) or soluble fiber (3 studies) and the risk of type 2 diabetes (44). Similar findings were reported in another meta-analysis of 18 prospective cohort studies in 617,968 participants (45). Higher versus lower intakes of total fiber were found to be associated with a 15% lower risk of type 2 diabetes (17 studies); the risk of type 2 diabetes was inversely related to the intake of cereal fiber (13 studies) and insoluble fiber (3 studies) but not related to the intake of fruit fiber (11 studies), vegetable fiber (11 studies), or soluble fiber (3 studies) (45). However, only randomized controlled interventions can establish whether there is a link of causality between an exposure (fiber intake) and an outcome (type 2 diabetes). For a discussion of the difference between observational studies and intervention studies, see the article "Epidemiological Studies" in the Spring/Summer LPI 2016 Research Newsletter.
Whole-grain cereals contain insoluble fibers, including cellulose, hemicellulose, and lignin. To date, intervention studies examining the effect of cereal fiber supplementation on the risk of type 2 diabetes are limited (46). In a randomized controlled study of 61 adults with metabolic syndrome, the consumption of a diet based on several whole-grain cereal products for 12 weeks had no effect on fasting plasma concentrations of glucose, insulin, or lipids, or on measures of insulin resistance compared with a refined grain-based diet (47). There was only some weak evidence of an effect of whole-grain cereals on postprandial insulin response (47). A recent 24-month, randomized, double-blind, placebo-controlled trial examined the effect of daily supplementation with 15 g of primarily insoluble fiber on glycemic control in 180 adults with impaired glucose tolerance who were counselled to adopt more healthy lifestyle habits. Insoluble fiber supplementation failed to improve fasting glucose concentration, measures of insulin sensitivity, HbA1c concentration (a marker of glycemic control), as well as glucose and insulin responses after a glucose load compared to placebo (25). Although observational data suggest a protective association of cereal fiber against type 2 diabetes, the current (yet limited) evidence from intervention trials does not support a role for insoluble fiber in glycemic control in individuals at risk of type 2 diabetes.
Fiber-related benefits on glucose homeostasis have been linked to the viscosity of certain soluble fibers (e.g., psyllium, β-glucan, raw guar gum) (see Improving glycemic control). Soluble viscous fibers in cereal, particularly β-glucans, rather than insoluble fiber (and soluble nonviscous fiber), are thus more likely to be involved in a protective effect of cereal intake against type 2 diabetes (48). Apart from fiber, other bioactive compounds in cereal, like magnesium, might contribute to improving glycemic control in people with impaired glucose tolerance (see the article on Magnesium) (49).
The current position of the American Diabetes Association is to encourage people at risk of type 2 diabetes to achieve the daily Adequate Intake (AI) of 14 g/1,000 kcal for dietary fiber (see Intake Recommendations) (50, 51). Adherence to a Mediterranean-style diet, the composition of which intends to meet the AI for fiber, has been associated with a lower risk of developing type 2 diabetes (52, 53).
Metabolic syndrome
Metabolic syndrome is estimated to affect nearly 35% of US adults and half of those older than 60 years (54). The term metabolic syndrome refers to a cluster of metabolic disorders that increase the risk of cardiovascular disease and type 2 diabetes mellitus. The diagnosis in an individual is based on the presence at once of at least three of the following metabolic risk factors: abdominal obesity, dyslipidemia, hypertension, impaired glucose tolerance/insulin resistance, and decreased blood HDL-cholesterol concentration. Two recent meta-analyses of observational studies have reported an inverse association between total fiber intake and odds of metabolic syndrome in cross-sectional studies but not in prospective cohort studies (55, 56).
Cancer
Numerous observational studies have examined the relationship between consumption of fiber and risk of cancer at various sites. A 2014 review compiled published analyses of data from the large, multicenter European Prospective Investigation into Cancer and Nutrition (EPIC) prospective cohort (>500,000 participants). This umbrella review reported evidence of inverse associations between higher versus lower daily total fiber intakes (≥28.5 g/day versus ≤16.4 g/day) and the risk of colorectal, liver, and breast cancers (57). Total fiber intakes were not associated with the risk of cancer at other sites, i.e., the biliary tract, endometrium, prostate, kidney, or bladder. In addition, further analyses suggested that the consumption of cereal fiber was inversely related to the risk of colorectal, stomach, and liver cancers, and vegetable fiber intake was inversely associated with breast cancer. Yet, associations between the consumption of specific fiber types were not examined in relation to the risk of endometrial, kidney, or bladder cancer in EPIC participants (57).
Pooling information from individual observational studies can be helpful to draw conclusions regarding the potential associations between dietary fiber consumption and cancer risk. Results from the most recent meta-analyses of observational studies are reported in Table 2.
| Type of Cancer | Type of Observational Studies | Risk Ratio [RR] or Odds Ratio [OR]* (95% Confidence Interval) | Risk Ratio [RR] in Subgroup Analyses (e.g., by fiber type, study type, and cancer subtype) | References |
|---|---|---|---|---|
| Breast cancer | 16 prospective cohort studies | RR: 0.93 (0.89-0.98) |
RR: 0.95 (0.86-1.06) in studies reporting on fruit fiber RR: 0.99 (0.92-1.07) in studies reporting on vegetable fiber RR : 0.96 (0.90-1.02) in studies reporting on cereal fiber RR: 0.91 (0.84-0.99) in studies reporting on soluble fiber RR: 0.95 (0.89-1.02) in studies reporting on insoluble fiber |
Aune et al. (2012) (75) |
| 20 prospective cohort and 4 case-control studies | RR: 0.88 (0.83-0.93) |
RR: 0.91 (0.87-0.95) in cohort studies only RR: 0.75 (0.47-1.02) in case-control studies only |
Chen et al. (2016) (76) | |
| Colorectal adenoma | 4 prospective cohort and 16 case-control studies | RR: 0.72 (0.63-0.83) |
RR: 0.84 (0.76-0.94) in studies reporting on fruit fiber RR: 0.93 (0.84-1.04) in studies reporting on vegetable fiber RR : 0.76 (0.62-0.92) in studies reporting on cereal fiber RR: 0.92 (0.76-1.10) in cohort studies only RR: 0.66 (0.56-0.77) in case-control studies only |
Ben et al. (2014) (58) |
| Colorectal cancer | 11 prospective cohort studies | RR: 0.86 (0.78-0.95) for proximal colorectal cancer |
RR: 0.93 (0.72-1.14) in women only RR: 0.79 (0.71-0.87) in men only |
Ma et al. (2018) (60) |
| RR: 0.79 (0.71-0.87) for distal colorectal cancer |
RR: 0.70 (0.52-0.87) in women only RR: 0.85 (0.74-0.95) in men only |
|||
| 13 prospective cohort and 8 case-control studies | RR: 0.74 (0.67-0.84) |
RR: 0.81 (0.74-0.89) in cohort studies only RR: 0.58 (0.50-0.68) in case-control studies only |
Gianfredi et al. (2018) (59) | |
| Endometrial cancer | 3 prospective cohort and 11 case-control studies | RR: 0.86 (0.73-1.02) |
RR: 1.22 (1.00-1.49) in cohort studies only OR: 0.76 (0.64-0.89) in case-control studies only RR: 1.26 (1.03-1.52) in studies reporting on cereal fiber OR: 0.74 (0.58-0.94) in studies reporting on vegetable fiber |
Chen et al. (2018) (83) |
| Esophageal cancer | 9 case-control studies |
OR: 0.66 (0.44-0.98) for esophageal adenocarcinoma OR: 0.61 (0.31-1.20) for esophageal squamous cell carcinoma |
Coleman et al. (2013) (84) | |
| 15 case-control studies | OR: 0.52 (0.43-0.64) |
OR: 0.42 (0.29-0.61) for Barrett’s esophagus (precancerous lesions) OR: 0.56 (0.37-0.67) for esophageal adenocarcinoma OR: 0.53 (0.31-0.90) for esophageal squamous cell carcinoma OR: 0.73 (0.48-1.12) in studies reporting on fruit fiber OR: 0.61 (0.45-0.83) in studies reporting on vegetable fiber OR : 0.81 (0.61-1.07) in studies reporting on cereal fiber OR: 0.85 (0.65-1.11) in studies reporting on grain fiber OR: 0.40 (0.20-0.78) in studies reporting on soluble fiber OR: 0.37 (0.18-0.75) in studies reporting on insoluble fiber |
Sun et al. (2017) (85) | |
| Gastric cancer | 2 prospective cohort and 19 case-control studies | OR: 0.58 (0.49-0.67) |
OR: 0.67 (0.46-0.99) in studies reporting on fruit fiber OR: 0.72 (0.57-0.90) in studies reporting on vegetable fiber OR: 0.58 (0.41-0.82) in studies reporting on cereal fiber OR: 0.41 (0.32-0.52) in studies reporting on soluble fiber OR: 0.42 (0.34-0.52) in studies reporting on insoluble fiber |
Zhang et al. (2013) (86) |
| Ovarian cancer | 5 prospective cohort and 14 case-control studies | RR: 0.70 (0.57-0.87) |
RR: 0.97 (0.85-1.12) in cohort studies RR: 0.62 (0.47-0.82) in case-control studies |
Xu et al. (2018) (87) |
| 4 prospective cohort and 13 case-control studies | RR: 0.76 (0.70-0.82) |
RR: 0.76 (0.63-0.92) in cohort studies RR: 0.75 (0.68-0.83) in case-control studies |
Huang et al. (2018) (88) | |
| Pancreatic cancer | 1 prospective cohort and 13 case-control studies | OR: 0.52 (0.43-0.63) |
OR: 1.01 (0.59-1.73) in the cohort study OR: 0.54 (0.44-0.67) in case-control studies |
Wang et al. (2015)** (89) |
| 1 prospective cohort and 13 case-control studies | OR: 0.52 (0.44-0.61) |
OR: 0.66 (0.51-0.80) in studies reporting on soluble fiber OR: 0.65 (0.44-0.87) in studies reporting on insoluble fiber |
Mao et al. (2017)** (90) | |
| Prostate cancer | 5 prospective cohort and 12 case-control studies | OR: 0.89 (0.77-1.01) |
OR: 0.94 (0.77-1.11) in cohort studies OR: 0.82 (0.68-0.96) in case-control studies OR: 0.92 (0.81-1.03) in studies reporting on fruit fiber OR: 0.87 (0.53-1.21) in studies reporting on vegetable fiber OR: 1.05 (0.94-1.16) in studies reporting on cereal fiber OR: 0.87 (0.52-1.22) in studies reporting on soluble fiber OR: 0.80 (0.46-1.13) in studies reporting on insoluble fiber |
Sheng et al. (2015) (91) |
| 5 prospective cohort and 11 case-control studies | RR: 0.94 (0.85-1.05) |
OR: 0.99 (0.87-1.14) in cohort studies OR: 0.89 (0.75-1.06) in case-control studies |
Wang et al. (2015) (92) | |
| Renal cell carcinoma | 2 prospective cohort and 4 case-control studies | RR: 0.84 (0.74-0.96) |
OR: 0.88 (0.69-1.12) in cohort studies OR: 0.82 (0.68-1.00) in case-control studies OR: 0.92 (0.80-1.05) in studies reporting on fruit fiber OR: 0.70 (0.49-1.00) in studies reporting on vegetable fiber OR: 1.04 (0.91-1.18) in studies reporting on cereal fiber OR: 0.83 (0.70-0.97) in studies reporting on soluble fiber OR: 0.81 (0.69-0.94) in studies reporting on insoluble fiber |
Huang et al. (2015) (93) |
|
*for the highest versus lowest level of fiber intake (unless otherwise specified) **both meta-analyses identified the same 14 observational studies |
||||
Colorectal cancer
Three most recent meta-analyses of observational studies have reported evidence of an inverse association between fiber intake and risk of colorectal cancer (see Table 2) (58-60). A recent review that included earlier meta-analyses reached a similar conclusion (61).
Several mechanisms have been proposed to explain why consuming fiber can have a protective effect against colorectal cancer. First, the presence of insoluble, coarse fiber can increase stool bulk thereby promoting the fecal excretion of carcinogens like nitrosamines (62). Fiber can also reduce exposure of the gut mucosa to carcinogens by shortening transit time (62). Secondly, fiber consumption influences the composition of the gut microbiota. In vitro studies have shown inulin to selectively stimulate the proliferation of beneficial bacteria while limiting the growth of potentially pathogenic bacteria (reviewed in 14). Gut bacterial imbalance (dysbiosis) has been associated with the incidence of several conditions, including colorectal cancer (63). The major health benefits conferred by the consumption of fiber are thus likely mediated by the bacteria the fiber contributes to feed. Depending on the physicochemical characteristics of fiber, some fiber, like inulin, can be fermented by colonic bacteria and lead to the formation of short-chain fatty acids, namely acetate, propionate, and butyrate. These short-chain fatty acids have been found to protect against gastrointestinal bacterial pathogens (64) and to display anti-inflammatory and anti-carcinogenic actions (65, 66).
A few controlled clinical trials have examined the effect of fiber consumption on the recurrence of colorectal adenomas (precancerous polyps), but none have been conducted in the last two decades. These trials examined the effect of wheat bran fiber (67-71), psyllium (72), and a high-fiber diet (73) on the risk of adenomas in participants with a history of adenomas. A 2017 meta-analysis of these trials found no difference between intervention and control groups in the number of participants with at least one new adenomatous polyp during the follow-up period (2-8 years), regardless of the type of fiber intervention (74).
Breast cancer
Dietary fiber might interfere with estrogen reabsorption by reducing β-glucoronidase activity (80). Alterations in gut bacteria composition have also been reported in women with breast cancer and might contribute to increased estrogen metabolism and absorption, resulting in higher circulating estrogen concentrations (81). However, it is not known whether fiber-associated effects on endogenous estrogen concentrations have a clinically significant impact on breast cancer risk (4). Finally, a healthy microbiota might also promote the degradation of plant-derived molecules other than fiber, such as lignans, which are precursors of metabolites with anti-estrogenic activities (82).
Other cancer sites
A review of the most recent meta-analyses of observational studies suggests that dietary fiber consumption is inversely associated with the risk of cancer of the esophagus (84, 85), stomach (86), pancreas (89, 90), and ovaries (see Table 2) (87, 88). The evidence linking fiber intake and esophageal cancer was exclusively based on observations from case-control studies, and for the other cancer sites, the evidence is primarily derived from case-control studies (Table 2). It is important to note that the evidence of an inverse association between fiber intake and risk of ovarian cancer (2 meta-analyses) was observed in case-control but not in prospective cohort studies (Table 2). Additionally, there was no evidence of an association between fiber intake and risk of endometrial cancer (1 meta-analysis; 83), prostate cancer (2 meta-analyses; 91, 92), or renal cell carcinoma (1 meta-analysis; 93) (Table 2). At present, evidence from randomized controlled trials of a causal relationship between fiber intake and risk of any cancer is lacking.
Of note, a recent study in a mouse model presenting a dysbiotic microbiota characterized by an increase in fiber-fermenting bacteria showed that the consumption of an obesogenic, high-fat diet enriched with soluble fiber could cause icteric hepatocarcinoma (94). Such findings suggest that a prolonged consumption of fermentable fiber may have detrimental consequences in contexts of dysbiosis. No such observations were found when insoluble fiber were substituted for soluble fiber (94).
Diarrhea associated with enteral nutrition
Gastrointestinal disorders associated with enteral nutrition prolong the time to recovery. A 2015 meta-analysis of 14 intervention studies found that fiber-enriched enteral formulas and/or fiber supplements reduced the overall incidence of diarrhea in patients requiring enteral nutrition (95). There was no reduction in incidental diarrhea when the analysis was restricted to studies that used prebiotic fiber (i.e., fermentable fiber influencing microbiota composition). Subgroup analyses also showed a benefit of fiber in non-critically ill patients but not in critically ill patients (95).
Fecal incontinence
A prospective cohort study that followed nearly 60,000 older women for four years found that the highest versus lowest level of fiber intake (mean, 25 g/day versus 13.5 g/day) was associated with a 17% lower risk of developing fecal incontinence (defined here as an incontinence episode of liquid or solid stool at least once a month) (96). A limited number of studies have also examined whether fiber supplementation might help treat established fecal incontinence. In one placebo-controlled trial, 206 subjects suffering from fecal incontinence were randomized for 32 days to receive fibers with different degrees of fermentability: gum arabic (on average, 16.6 g/day; highly fermentable), sodium carboxymethylcellulose (16.2 g/day; partially fermentable), and psyllium (14.6 g/day; poorly fermentable) (97). The frequency of fecal incontinence increased with sodium carboxymethylcellulose but decreased with gum arabic and psyllium compared to placebo. Stool consistency and amount did not differ among groups (97). A randomized, cross-over trial in 80 community-dwelling participants with at least one fecal incontinence episode per week found that the reduction in fecal incontinence frequency and severity with psyllium supplementation was equivalent to that observed with antidiarrheal drug loperamide (Imodium) (98).
Weight control
It has been suggested that higher fiber intakes could help maintain weight or promote weight loss by increasing satiation (causing meal termination) and/or extending the feeling of fullness after a meal (satiety). Several mechanisms have been proposed to explain the potential satiating effect of fibers and the subsequent reduction in food intake. The presence of fiber in food may indirectly stimulate the production of hormones involved in the regulation of appetite in particular through (i) increasing the processing time in the mouth due to increased efforts required to masticate large particles containing fibers, and/or (ii) increasing the duration of stomach distention due to a lower rate of gastric emptying, and/or (iii) increasing the colonic production of short-chain fatty acids that can bind to receptors present on gut endocrine cells (reviewed in 99). Adverse effects like gas production and bloating observed with the supplementation of isolated fibers (e.g., wheat dextrin) might also reduce hunger and increase satiety.
A 2013 review of 44 randomized controlled trials found that β-glucans from oat or barley, lupin kernel fiber, whole grain rye, rye bran, and a mixed high-fiber diet could enhance satiety, whereas psyllium, whole grain barley, whole grain buckwheat, resistant starch, and wheat bran had no benefit or even reduced measures of satiety (100). However, for many types of fiber examined, results from interventions were mixed, some showing a positive effect on satiety, and others showing no effect. Additionally, there seemed to be no relationship between the physicochemical properties of fiber (i.e., solubility, viscosity, fermentability) and evidence of efficacy. For example, among soluble viscous fibers, β-glucans appeared to enhance satiety, but pectin or psyllium did not. Similarly, among fermentable fibers, β-glucans enhanced satiety, but guar gum, inulin, fructooligosaccharides, and resistant starch did not. Finally, a positive effect of fiber on satiety was not consistently associated with a reduction in food intake (100).
A 2011 systematic review of 61 randomized controlled studies examined the effect of different fiber types on body weight (101). This analysis found that dextrins and marine polysaccharides reduced body weight in all the studies, while chitosan, arabinoxylans, and fructans reduced body weight in at least two-thirds of the studies. Average weight reductions were greatest for the fructans and marine polysaccharides groups (~1.3 kg or 2.8 lb/4 weeks for a 79 kg person in both groups). For all fiber types combined, however, the average weight reduction was only 0.3 kg (0.7 lb) per 4 weeks for a 79-kg person (101). A few randomized controlled trials in overweight or obese subjects suggested that psyllium supplementation may influence body composition and/or promote weight loss (reviewed in 102). In one randomized, placebo-controlled trial in 159 Australian with body mass indices (BMI) ≥25 kg/m2, psyllium (5 g/day) reduced waist circumference, waist-to-hip ratio, and body fat percentage, and increased the percentage of lean mass after 3, 6, and 12 months (103). Psyllium appeared to transiently reduce body weight at 3 and 6 months, yet there was no difference in body weight between psyllium and placebo at the end of the intervention (12 months) (103).
More research needs to be conducted in order to clarify which types of fiber might play a role in appetite regulation and weight management (99).
Mortality
Several prospective cohort studies have examined dietary fiber intake in relation to all-cause and cause-specific mortality. A 2015 report from the NIH-AARP Diet and Health Study, which followed 364,442 older adults for an average of 14 years, found that men and women in the highest versus lowest quintile of dietary fiber intake (mean, 10.2 g/day versus 2.0 g/day) had lower risks of all-cause mortality (-19%) and mortality from cardiovascular disease (-20%), cancer (-15%), diabetes mellitus (-34%), and respiratory diseases (-21%) (104). Another prospective study that made use of data collected from 15,740 participants in the US National Health and Nutrition Examination Survey (NHANES) 1988-1994 found a 13% lower risk of all-cause mortality in subjects with total fiber intake between 14.5 g/day and 22.1 g/day — but not in those with higher intake (>22.1 g/day) — compared to those with fiber intake less than 9.3 g/day, over a mean follow-up period of 13.7 years (105). No associations were found between intakes of either insoluble or soluble fiber and all-cause mortality (105).
A meta-analysis of prospective cohort studies published before 2013, which included a total of 1,752,848 participants followed for a mean 12.4 years, found higher versus lower total fiber intake to be associated with lower risks of all-cause mortality (-23%; 9 studies), cancer-related mortality (-17%; 5 studies), and cardiovascular disease-related mortality (-23%; 16 studies) (106). Another meta-analysis identified 14 prospective cohort studies that examined cereal fiber intake in relation to mortality (107). Participants in the highest versus lowest quartile of cereal fiber intake had lower risks of all-cause mortality (-19%; 3 studies), cardiovascular disease-related mortality (-18%; 10 studies), and cancer-related mortality (-25%; 2 studies) (107).
Disease Treatment
Diabetes mellitus
A 2004 meta-analysis that combined the results of 23 clinical trials in patients with type 1 or type 2 diabetes mellitus found that high-fiber diets (≥20 g/1,000 kcal) lowered postprandial blood glucose concentrations by 13%-21%, serum LDL cholesterol concentrations by 8%-16%, and serum triglyceride concentrations by 8%-13% when compared with low-fiber diets (<10 g/1,000 kcal) (108). Based on the evidence from this meta-analysis, the authors recommended a dietary fiber intake of 25-50 g/day (15-25 g/1,000 kcal) for individuals with diabetes, which is slightly higher than recommendations for the general public (14 g/1,000 kcal) (4). However, recommendations from the American Diabetes Association and the Academy of Nutrition and Dietetics to people with diabetes are similar to those prescribed for the population as a whole (50, 109).
Adhering to one of the USDA’s healthy dietary patterns, like the Mediterranean-style diet (which is rich in fruit, vegetables, and whole grains), would contribute to meeting the daily intake recommendation for total fiber (see Intake Recommendations) (110). A 2015 meta-analysis of nine randomized controlled trials in a total of 1,178 participants with type 2 diabetes showed evidence of body weight loss and improvements in glycemic control and blood lipid profile with the consumption of a Mediterranean-style diet compared to a control diet (111).
Numerous controlled clinical trials have shown that supplementation with soluble viscous fibers improves markers of glycemic control in people who have type 2 diabetes mellitus. A meta-analysis of 28 trials in 1,394 adults with type 2 diabetes found reductions in HbA1c concentration (20 trials), fasting glucose concentration (28 trials), and insulin resistance (11 trials) with soluble viscous fiber supplementation (median doses of 10.5-15 g/day for 6-8 weeks) (112). Another meta-analysis of 35 trials showed that the effect of psyllium varied with baseline fasting glucose concentration: psyllium supplementation had no effect on markers of glycemic control in euglycemic participants but showed a modest benefit in subjects with impaired glucose tolerance, and a greater effect in those with overt type 2 diabetes (see also Biological Activities) (32).
A small randomized uncontrolled trial in 20 healthy participants suggested that supplemental wheat dextrin, which is partially absorbed as sugar in the small intestine, could increase fasting glucose concentration into the prediabetes range after one month of supplementation (113). Since there is little evidence from clinical trials that increasing nonviscous fiber alone is beneficial (114), individuals with diabetes should preferably increase fiber intake from sources of soluble viscous fibers, such as oats and barley (β-glucans), vegetables, beans, and legumes (108).
Gastrointestinal disorders
Chronic idiopathic constipation
Only insoluble fibers and soluble viscous fibers that resist bacterial fermentation in the colon have a potential laxative effect (see Improving regularity in stool elimination) (15). The prevalence of chronic constipation is higher among people with diabetes mellitus, in women during pregnancy and after delivery, or in older people. The management of constipation in these patients is usually similar to the management in the rest of the population, although the etiology might be different. Bulk-forming laxatives, including psyllium, bran, and methylcellulose, are commonly recommended to improve stool regularity in patients with diabetes mellitus (115). However, there is no evidence that methylcellulose and bran are efficacious in patients with constipation (116). In these patients, psyllium is also recognized to improve glycemic control (see Diabetes mellitus). There is a need for good quality, randomized, double-blind, controlled trials to examine the effect of fiber supplementation in the treatment of constipation in older adults in long-term care (117) or in pregnant women and new mothers (118, 119).
The American College of Gastroenterology recognizes the efficacy of soluble fiber in the treatment of chronic idiopathic constipation. It also recognizes that the evidence from observational studies is mixed, as constipation is associated with low-fiber diets in some, but not all, studies (120). It recommends a gradual increase in fiber intake, in particular to limit the potential adverse effects associated with the intake of insoluble fiber, i.e., bloating, distension, flatulence, and cramping (121).
Irritable bowel syndrome
Irritable bowel syndrome (IBS) is a functional disorder of the intestines, characterized by episodes of abdominal pain or discomfort associated with altered gut mobility and changes in bowel habits (i.e., with constipation, diarrhea, or both) (122). Although the pathophysiology of IBS remains unclear, certain food components have been recognized as a cause for symptoms of IBS. Dietary restriction of highly fermentable, soluble, short-chain carbohydrates, identified as FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) and including some dietary fibers (e.g., fructans, galactooligosaccharides), has been found to relieve IBS symptoms, including abdominal pain/discomfort, abdominal bloating/distension, and flatulence (123). On the other hand, soluble, poorly fermentable, long-chain carbohydrate fiber types may improve the symptoms related to excessive gas production. Two meta-analyses of randomized controlled trials and cross-over studies found a beneficial effect of fiber that was limited to soluble fiber, primarily psyllium (124, 125). Accordingly, the American College of Gastroenterology recognizes that soluble fiber like psyllium can provide overall symptom relief in IBS, while insoluble fiber (e.g., wheat bran) can cause bloating and abdominal discomfort (121). More research is needed to document the effect of specific soluble fibers, considering physicochemical properties (viscosity and fermentability), doses, and duration of supplementation, and to provide stronger recommendations to individuals diagnosed with IBS (125). Future trials should also consider subjects with all of the IBS types, i.e., constipation-predominant, diarrhea-predominant, and mixed-diarrhea-and-constipation IBS.
Diverticular disease
Diverticular disease or diverticulosis is a rather common gastrointestinal condition in Western countries characterized by the formation of small pouches (diverticula) in the colon (126). Acute inflammation or infection of diverticula — known as diverticulitis — occurs in about 10%-25% of all symptomatic cases of diverticulosis and is caused by the irritation of the mucosa by fecalith obstructing diverticula. Complications of diverticulitis include abscesses, fistulas, obstruction, and perforation (126). The etiology of diverticulosis is thought to be multifactorial, involving both genetic and environmental risk factors. Despite little supporting evidence, it has been proposed that low fiber intakes that characterize Western diets might contribute to increasing the risk of diverticulosis (127, 128). This low-fiber hypothesis is disputed. In particular, a 2012 cross-sectional study of 2,104 adults found higher odds of diverticula (assessed by colonoscopy) among participants in the highest versus lowest quartile of fiber intake, measured by food frequency questionnaires (129).
A 2017 review identified interventions — published over four decades — that examined the effect of dietary or supplemental fiber on the reduction of abdominal pain in patients suffering from symptomatic uncomplicated diverticular disease (SUDD), as well as on the risk of acute diverticulitis (130). However, a meta-analysis could not be conducted nor any conclusion provided regarding the efficacy of fiber in the treatment of SUDD due to the very poor quality of the studies and their substantial heterogeneity in terms of study design and quantity and quality of fiber types used (130). Another recent review of the literature focused on the effect of fiber-restricted diets in the management of acute uncomplicated diverticulitis (131). Based on the review of three randomized controlled trials and two observational studies, the authors found a reduced length of hospital stay with non-restricted diets compared to restricted diets, but no difference regarding the incidence of treatment failure (i.e., the risk of no clinical improvement with therapy and the development of complications) and the risk of post-discharge reoccurrence of diverticulitis. While there appears to be no clinical benefit in restricting fiber intake in subjects with uncomplicated diverticulitis, the quality of the studies was once again deemed to be very low (131).
Despite the lack of high-quality evidence regarding the potential benefit of fiber in the management of diverticular disease, many national guidelines recommend the use of high-fiber diets in patients with SUDD and for the prevention of diverticulitis (132, 133).
Hemorrhoids
A limited number of interventions have examined the effect of fiber supplementation in subjects with symptomatic hemorrhoids. A randomized controlled trial in 67 participants found that supplementation with psyllium (7 g/day for 6 weeks) improved stool consistency and regularity, reduced the use of laxatives, and increased the quality of life compared to a placebo (134). Another randomized controlled trial in 50 patients with hemorrhoidal prolapse (grades II-IV) and rectal bleeding showed that psyllium supplementation (11.6 g/day for 40 days) reduced the number of bleeding episodes and the number of congested hemorrhoidal cushions but had no effect on the degree of prolapse (135). Finally, a more recent uncontrolled intervention in 102 individuals with advanced hemorrhoids (grades II-IV) examined the effect of counseling patients to follow a therapy meant to improve defecatory habits and involving an increase of psyllium intake to 20 g/day-25 g/day. A follow-up for a median 40 months suggested that psyllium supplementation might help halt the progression of hemorrhoidal prolapse and reduce the number of bleeding episodes (136).
Sources
Food sources
An analysis of the 2009-2010 US National Health and Nutrition Examination Survey (NHANES) data reported average dietary fiber intakes of 13.6 g/day in children and adolescents and 17 g/day in adults—well below recommended intake levels (see Intake Recommendations) (137). Fiber is identified as a shortfall nutrient of public health concern in the 2010-2015 Dietary Guidelines for Americans (51).
Good sources of dietary fiber include legumes, nuts, whole grains, bran products, fruit, and nonstarchy vegetables. Legumes (e.g., dry beans and peas), nuts, seeds, and whole grains are generally more concentrated sources of fiber than fruit and vegetables (138). These higher fiber foods are currently underconsumed, contributing to only about 6% of total dietary fiber intake (137). Although refined grains are often perceived as being poor sources of fiber, they can provide as much fiber as either fruit or vegetables when comparable serving sizes are consumed (138). In addition, not all whole grains are good sources of fiber, yet they provide key micronutrients and phytochemicals that contribute to the health benefit associated with whole grain consumption (see the article on Whole Grains) (12).
All plant-based foods contain a mixture of soluble and insoluble fiber (138). Bran flaxseed, oat cereal, legumes, nuts, fruit, and vegetables are good sources of soluble viscous and nonviscous fiber. Wheat bran, brown rice, barley, cabbage, celery, and whole grains are rich sources of insoluble fiber. The total fiber content of some fiber-rich foods is presented in Table 3. Some strategies for increasing dietary fiber intake include increasing fruit and nonstarchy vegetable intake, increasing intake of legumes, eating whole-grain cereal or oatmeal for breakfast, substituting whole grains for refined grains, and substituting nuts or popcorn for less healthy snacks. For more information about the fiber content of specific foods, search USDA's FoodData Central database.
Isolated fibers and supplements
β-Glucans
β-Glucans are viscous, easily fermented, soluble fibers found naturally in oats, barley, mushrooms, yeast, bacteria, and algae. β-Glucans extracted from oats, mushrooms, and yeast are available in a variety of nutritional supplements without a prescription.
Glucomannan
Glucomannan, sometimes called konjac mannan, is classified as a soluble fiber isolated from konjac flour, which is derived from the plant Amorphophallus konjac. Glucomannan is available as powder and in capsules, which should be taken with plenty of liquids (8). Glucomannan forms gels that are firmer than regular gelatin products (e.g., "jello") and do no melt in the mouth. The FDA has banned gel candies containing glucomannan (e.g., "mini-cup jelly products") because of their potential to cause choking (139).
Pectin
Pectins are readily fermented soluble viscous fibers, most often extracted from citrus peels and apple pulp. Pectins are widely used as gelling agents in food but are also available as dietary supplements without a prescription (8).
Inulins and oligofructose
Inulins and oligofructose, extracted from chicory root or synthesized from sucrose, are used as food additives (9). Isolated inulin is added to replace fat in products like salad dressing, while sweet-tasting oligofructose is added to products like fruit yogurts and desserts. Inulins and oligofructose are highly fermentable fibers that are also classified as prebiotics because of their ability to stimulate the growth of potentially beneficial Bifidobacteria species in the human colon (140). Encouraging the growth of Bifidobacteria might promote intestinal health by suppressing the growth of pathogenic bacteria known to cause diarrhea or by enhancing the immune response (141). Although a number of dietary supplements containing inulins and oligofructose are marketed as prebiotics, the health benefits of prebiotics have not yet been convincingly demonstrated in humans (11, 142).
Guar gum
Raw guar gum is a viscous, fermentable fiber derived from the Indian guar or cluster bean (4). It is used as a thickener or emulsifier in many food products. Dietary supplements containing guar gum have been marketed as weight-loss aids, but there is no evidence of their efficacy (143). Unlike guar gum, partially hydrolyzed guar gum is nonviscous and therefore does not exhibit the biological activities of guar gum (i.e., it has no effect on serum cholesterol and glycemic control) (see Biological Activities).
Psyllium
Psyllium, a viscous, soluble, gel-forming fiber isolated from psyllium seed husks, is available without a prescription in laxatives, ready-to-eat cereal, and dietary supplements (8). Psyllium is proven to be efficacious to lower serum cholesterol and improve glycemic control (see Biological Activities). Because it also normalizes stool form, psyllium is the only fiber recommended by the American College of Gastroenterology to treat chronic constipation and irritable bowel syndrome (see Gastrointestinal disorders).
Chitosan
Chitosan is an indigestible glucosamine polymer derived from chitin. Chitosan is available as a dietary supplement without a prescription in the US, being marketed to promote weight loss and lower cholesterol. A 2018 meta-analysis of randomized controlled, clinical trials found a lowering of total and LDL-cholesterol concentrations with chitosan supplementation (0.3-6.75 g/day for 4-24 weeks) and no effect on HDL-cholesterol or triglycerides (144). Another recent pooled analysis of trials found chitosan to be more effective than placebo in promoting weight loss (145).
Note: All fiber supplements should be taken with sufficient fluids. Most clinicians recommend taking fiber supplements with at least 8 ounces (240 mL) of water and consuming a total of at least 64 ounces (~2 liters or 2 quarts) of fluid daily (146, 147).
Safety
Adverse effects
Dietary fiber
Some people experience abdominal cramping, bloating, or gas when they abruptly increase their dietary fiber intake (146, 147). These symptoms can be minimized or avoided by increasing intake of fiber-rich foods gradually and increasing fluid intake to at least 64 oz/day (~2 liters or 2 quarts/day). There have been rare reports of intestinal obstruction related to large intakes of oat bran or wheat bran, primarily in people with impaired intestinal motility or difficulty chewing (148-151). The National Academy of Medicine (formerly, the Institute of Medicine) has not established a tolerable upper intake level (UL) for dietary or functional fiber (4).
Isolated fibers and fiber supplements
Gastrointestinal symptoms: The following fibers have been found to cause gastrointestinal distress, including abdominal cramping, bloating, gas, and diarrhea: guar gum, inulin and oligofructose, fructooligosaccharides, polydextrose, resistant starch, and psyllium (4). It is recommended to gradually introduce a new fiber supplement, not exceeding 3 to 4 g/day the first week, in order to minimize gastrointestinal symptoms (152). In subjects who are constipated, the initiation of a fiber supplement should start once the hard stool is cleared (152). Use of a guar gum-containing supplement for weight loss has been associated with esophageal and small bowel obstruction (153). Additionally, several cases of intestinal obstruction by psyllium have been reported when taken with insufficient fluids or by people with impaired swallowing or gastrointestinal motility (154, 155).
Colorectal adenomas: One randomized controlled trial in patients with a history of colorectal adenomas (precancerous polyps) found that supplementation with 3.5 g/day of psyllium for three years resulted in a significant increase in colorectal adenoma recurrence compared to placebo (see Colorectal cancer) (72).
Allergy and anaphylaxis: Since chitin is isolated from the exoskeletons of crustaceans, such as crabs and lobsters, and chitosan is derived from chitin, people with shellfish allergies should avoid taking chitosan supplements (8). Anaphylaxis has been reported after intravenous (IV) administration of inulin (156), as well as ingestion of margarine containing inulin extracted from chicory (157). Anaphylaxis has also been reported after the ingestion of cereal containing psyllium, and asthma has occasionally been reported in people with occupational exposure to psyllium powder (158).
Drug interactions
Gel-forming fibers (e.g., β-glucan, psyllium, raw guar gum, pectin) have the potential to slow the absorption of drugs if taken at the same time. Psyllium may reduce the absorption of lithium, carbamazepine (Tegretol), digoxin (Lanoxin), and warfarin (Coumadin) when taken at the same time (8). Guar gum may slow the absorption of digoxin, acetaminophen (Tylenol), and bumetanide (Bumex) and decrease the absorption of metformin (Glucophage), penicillin, and some formulations of glyburide (Glynase) when taken at the same time (159). Pectin may decrease the absorption of lovastatin (Mevacor) when taken at the same time (160). Concomitant administration of a kaolin-pectin antidiarrheal suspension has been reported to decrease the absorption of clindamycin, tetracycline, and digoxin, but it is not known whether kaolin, pectin, or both were responsible for the interaction (8). In general, medications should be taken at least one hour before or two hours after fiber supplements and gel-forming dietary fibers (e.g., oatmeal).
Nutrient interactions
The addition of cereal fiber to meals has generally been found to decrease the absorption of iron, zinc, calcium, and magnesium in the same meal, but this effect appears to be related to the phytate present in the cereal fiber rather than the fiber itself (161). In general, dietary fiber as part of a balanced diet has not been found to adversely affect the calcium, magnesium, iron, or zinc status of healthy people at recommended intake levels (4). Evidence from animal studies and limited research in humans suggests that inulin and oligofructose may enhance calcium absorption (162, 163). The addition of pectin and guar gum to a meal significantly reduced the absorption of the carotenoids β-carotene, lycopene, and lutein from that meal (164, 165).
Intake Recommendations
The Adequate Intake (AI) for total fiber
The Adequate Intake (AI) recommendations for total fiber intake, set by the Food and Nutrition Board of the Institute of Medicine, are based on the findings of several large prospective cohort studies that dietary fiber intakes of approximately 14 g for every 1,000 calories (kcal) consumed were associated with significant reductions in the risk of coronary heart disease (CHD). The FDA approved specific health claims related to the cardioprotective effects of two soluble, gel-forming fibers only: β-glucan and psyllium (see Disease Prevention). For adults who are 50 years of age and younger, the AI recommendation for total fiber intake is 38 g/day for men and 25 g/day for women. For adults over 50 years of age, the recommendation is 30 g/day for men and 21 g/day for women. The AI recommendations for males and females of all ages are presented in Table 4 (4).
Some suggestions for increasing fiber intake
- Eat at least five servings of fruit and vegetables daily (see the article on Fruit and Vegetables).
- Substitute whole grains for refined grains (see the article on Whole Grains).
- Eat oatmeal, whole-grain cereal, or bran cereal for breakfast.
- Eat beans, split peas, or lentils at least once weekly (see the article on Legumes).
- Substitute nuts or popcorn for less healthful snacks like potato chips or candy (see the article on Nuts).
Adopting one of the USDA healthy dietary patterns (i.e., healthy US-style, healthy Mediterranean-style, and healthy vegetarian dietary patterns) recommended in the 2015-2020 Dietary Guidelines for Americans will help meet the recommendations for total fiber intake (110). Fruit, vegetables, and whole grains available in the USDA dietary patterns contribute nearly 90% of the recommended dietary fiber intake. Within the vegetable group, beans, peas, and starchy vegetables are the main contributor of total fiber intake (22%). Refined grains provide 9% of total fiber intake (110).
Authors and Reviewers
Originally written in 2004 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in December 2005 by:
Jane Higdon, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in August 2009 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in April 2012 by:
Victoria J. Drake, Ph.D.
Linus Pauling Institute
Oregon State University
Updated in March 2019 by:
Barbara Delage, Ph.D.
Linus Pauling Institute
Oregon State University
Reviewed in June 2019 by:
Johnson W. McRorie, Jr., Ph.D., F.A.C.G., A.G.A.F., F.A.C.N.
Procter & Gamble
Mason, OH
Copyright 2004-2025 Linus Pauling Institute
References
1. Lupton JR. Microbial degradation products influence colon cancer risk: the butyrate controversy. J Nutr. 2004;134(2):479-482. (PubMed)
2. Ha MA, Jarvis MC, Mann JI. A definition for dietary fibre. Eur J Clin Nutr. 2000;54(12):861-864. (PubMed)
3. DeVries JW. On defining dietary fibre. Proc Nutr Soc. 2003;62(1):37-43. (PubMed)
4. Institute of Medicine. Dietary, functional, and total fiber. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, D. C.: The National Academies Press; 2002:265-334. (The National Academies Press)
5. Trowell H. Dietary fibre, ischaemic heart disease and diabetes mellitus. Proc Nutr Soc. 1973;32(3):151-157. (PubMed)
6. Lupton JR, Turner ND. Dietary fiber. In: Stipanuk MH, ed. Biochemical and Physiological Aspects of Human Nutrition. Philadelphia: W. B. Saunders; 2000:143-154.
7. Gallaher CM, Schneeman BO. Dietary fiber. In: Bowman BA, Russell RM, eds. Present Knowledge in Nutrition. 8th ed. Washington, D.C.: ILSI Press; 2001:83-91.
8. Hendler SS, Rorvik DR, eds. PDR for Nutritional Supplements. 2nd ed. Montvale: Physicians' Desk Reference Inc.; 2008.
9. Niness KR. Inulin and oligofructose: what are they? J Nutr. 1999;129(7 Suppl):1402S-1406S. (PubMed)
10. Wilson B, Whelan K. Prebiotic inulin-type fructans and galacto-oligosaccharides: definition, specificity, function, and application in gastrointestinal disorders. J Gastroenterol Hepatol. 2017;32 Suppl 1:64-68. (PubMed)
11. McRorie JW, Jr. Evidence-based approach to fiber supplements and clinically meaningful health benefits, part 1: what to look for and how to recommend an effective fiber therapy. Nutr Today. 2015;50(2):82-89. (PubMed)
12. Dahl WJ, Stewart ML. Position of the Academy of Nutrition and Dietetics: health implications of dietary fiber. J Acad Nutr Diet. 2015;115(11):1861-1870. (PubMed)
13. Holscher HD. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. 2017;8(2):172-184. (PubMed)
14. Zeng H, Lazarova DL, Bordonaro M. Mechanisms linking dietary fiber, gut microbiota and colon cancer prevention. World J Gastrointest Oncol. 2014;6(2):41-51. (PubMed)
15. McRorie JW, Jr., McKeown NM. Understanding the physics of functional fibers in the gastrointestinal tract: an evidence-based approach to resolving enduring misconceptions about insoluble and soluble fiber. J Acad Nutr Diet. 2017;117(2):251-264. (PubMed)
16. Wei ZH, Wang H, Chen XY, et al. Time- and dose-dependent effect of psyllium on serum lipids in mild-to-moderate hypercholesterolemia: a meta-analysis of controlled clinical trials. Eur J Clin Nutr. 2009;63(7):821-827. (PubMed)
17. Brum J, Ramsey D, McRorie J, Bauer B, Kopecky SL. Meta-analysis of usefulness of psyllium fiber as adjuvant antilipid therapy to enhance cholesterol lowering efficacy of statins. Am J Cardiol. 2018;122(7):1169-1174. (PubMed)
18. Jovanovski E, Yashpal S, Komishon A, et al. Effect of psyllium (Plantago ovata) fiber on LDL cholesterol and alternative lipid targets, non-HDL cholesterol and apolipoprotein B: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2018;108(5):922-932. (PubMed)
19. Sniderman AD, Williams K, Contois JH, et al. A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes. 2011;4(3):337-345. (PubMed)
20. Ho HV, Sievenpiper JL, Zurbau A, et al. A systematic review and meta-analysis of randomized controlled trials of the effect of barley beta-glucan on LDL-C, non-HDL-C and apoB for cardiovascular disease risk reduction(i-iv). Eur J Clin Nutr. 2016;70(11):1239-1245. (PubMed)
21. Ho HV, Sievenpiper JL, Zurbau A, et al. The effect of oat beta-glucan on LDL-cholesterol, non-HDL-cholesterol and apoB for CVD risk reduction: a systematic review and meta-analysis of randomised-controlled trials. Br J Nutr. 2016;116(8):1369-1382. (PubMed)
22. Ho HVT, Jovanovski E, Zurbau A, et al. A systematic review and meta-analysis of randomized controlled trials of the effect of konjac glucomannan, a viscous soluble fiber, on LDL cholesterol and the new lipid targets non-HDL cholesterol and apolipoprotein B. Am J Clin Nutr. 2017;105(5):1239-1247. (PubMed)
23. Kerckhoffs DA, Hornstra G, Mensink RP. Cholesterol-lowering effect of beta-glucan from oat bran in mildly hypercholesterolemic subjects may decrease when beta-glucan is incorporated into bread and cookies. Am J Clin Nutr. 2003;78(2):221-227. (PubMed)
24. Food and Drug Administration. Electronic Code of Federal Regulations. Health claims: Soluble fiber from certain foods and risk of coronary heart disease (Title 21, Chapter I, Subchapter B, Part 101, Subpart E, §101.81). 9th April 2018. Available at: https://www.ecfr.gov/cgi-bin/text-idx?SID=f76b9be8e71b67f3483005802c386205&mc=true&node=se21.2.101_181&rgn=div8. Accessed 3/7/19.
25. Honsek C, Kabisch S, Kemper M, et al. Fibre supplementation for the prevention of type 2 diabetes and improvement of glucose metabolism: the randomised controlled Optimal Fibre Trial (OptiFiT). Diabetologia. 2018;61(6):1295-1305. (PubMed)
26. Schafer G, Schenk U, Ritzel U, Ramadori G, Leonhardt U. Comparison of the effects of dried peas with those of potatoes in mixed meals on postprandial glucose and insulin concentrations in patients with type 2 diabetes. Am J Clin Nutr. 2003;78(1):99-103. (PubMed)
27. Kabir M, Oppert JM, Vidal H, et al. Four-week low-glycemic index breakfast with a modest amount of soluble fibers in type 2 diabetic men. Metabolism. 2002;51(7):819-826. (PubMed)
28. Brand-Miller JC, Atkinson FS, Gahler RJ, Kacinik V, Lyon MR, Wood S. Effects of PGX, a novel functional fibre, on acute and delayed postprandial glycaemia. Eur J Clin Nutr. 2010;64(12):1488-1493. (PubMed)
29. Jenkins AL, Kacinik V, Lyon MR, Wolever TM. Reduction of postprandial glycemia by the novel viscous polysaccharide PGX, in a dose-dependent manner, independent of food form. J Am Coll Nutr. 2010;29(2):92-98. (PubMed)
30. Sierra M, Garcia JJ, Fernandez N, Diez MJ, Calle AP, Sahagun AM. Effects of ispaghula husk and guar gum on postprandial glucose and insulin concentrations in healthy subjects. Eur J Clin Nutr. 2001;55(4):235-243. (PubMed)
31. Williams JA, Lai CS, Corwin H, et al. Inclusion of guar gum and alginate into a crispy bar improves postprandial glycemia in humans. J Nutr. 2004;134(4):886-889. (PubMed)
32. Gibb RD, McRorie JW, Jr., Russell DA, Hasselblad V, D'Alessio DA. Psyllium fiber improves glycemic control proportional to loss of glycemic control: a meta-analysis of data in euglycemic subjects, patients at risk of type 2 diabetes mellitus, and patients being treated for type 2 diabetes mellitus. Am J Clin Nutr. 2015;102(6):1604-1614. (PubMed)
33. Bodnaruc AM, Prud'homme D, Blanchet R, Giroux I. Nutritional modulation of endogenous glucagon-like peptide-1 secretion: a review. Nutr Metab (Lond). 2016;13:92. (PubMed)
34. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. (PubMed)
35. Khan K, Jovanovski E, Ho HVT, et al. The effect of viscous soluble fiber on blood pressure: A systematic review and meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis. 2018;28(1):3-13. (PubMed)
36. McRorie JW, Chey WD. Fermented fiber supplements are no better than placebo for a laxative effect. Dig Dis Sci. 2016;61(11):3140-3146. (PubMed)
37. Christodoulides S, Dimidi E, Fragkos KC, Farmer AD, Whelan K, Scott SM. Systematic review with meta-analysis: effect of fibre supplementation on chronic idiopathic constipation in adults. Aliment Pharmacol Ther. 2016;44(2):103-116. (PubMed)
38. Wolk A, Manson JE, Stampfer MJ, et al. Long-term intake of dietary fiber and decreased risk of coronary heart disease among women. JAMA. 1999;281(21):1998-2004. (PubMed)
39. Rimm EB, Ascherio A, Giovannucci E, Spiegelman D, Stampfer MJ, Willett WC. Vegetable, fruit, and cereal fiber intake and risk of coronary heart disease among men. JAMA. 1996;275(6):447-451. (PubMed)
40. Pietinen P, Rimm EB, Korhonen P, et al. Intake of dietary fiber and risk of coronary heart disease in a cohort of Finnish men. The Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Circulation. 1996;94(11):2720-2727. (PubMed)
41. Threapleton DE, Greenwood DC, Evans CE, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2013;347:f6879. (PubMed)
42. Wu Y, Qian Y, Pan Y, et al. Association between dietary fiber intake and risk of coronary heart disease: A meta-analysis. Clin Nutr. 2015;34(4):603-611. (PubMed)
43. Ning H, Van Horn L, Shay CM, Lloyd-Jones DM. Associations of dietary fiber intake with long-term predicted cardiovascular disease risk and C-reactive protein levels (from the National Health and Nutrition Examination Survey Data [2005-2010]). Am J Cardiol. 2014;113(2):287-291. (PubMed)
44. Yao B, Fang H, Xu W, et al. Dietary fiber intake and risk of type 2 diabetes: a dose-response analysis of prospective studies. Eur J Epidemiol. 2014;29(2):79-88. (PubMed)
45. InterAct Consortium. Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct Study and a meta-analysis of prospective studies. Diabetologia. 2015;58(7):1394-1408. (PubMed)
46. Whincup PH, Donin AS. Cereal fibre and type 2 diabetes: time now for randomised controlled trials? Diabetologia. 2015;58(7):1383-1385. (PubMed)
47. Giacco R, Costabile G, Della Pepa G, et al. A whole-grain cereal-based diet lowers postprandial plasma insulin and triglyceride levels in individuals with metabolic syndrome. Nutr Metab Cardiovasc Dis. 2014;24(8):837-844. (PubMed)
48. Gemen R, de Vries JF, Slavin JL. Relationship between molecular structure of cereal dietary fiber and health effects: focus on glucose/insulin response and gut health. Nutr Rev. 2011;69(1):22-33. (PubMed)
49. McRae MP. Dietary fiber Intake and type 2 diabetes mellitus: an umbrella review of meta-analyses. J Chiropr Med. 2018;17(1):44-53. (PubMed)
50. Bantle JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31 Suppl 1:S61-78. (PubMed)
51. US Department of Health and Human Services/ US Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. Available at: https://health.gov/dietaryguidelines/2015/. Accessed 3/18/19.
52. Medina-Remon A, Kirwan R, Lamuela-Raventos RM, Estruch R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit Rev Food Sci Nutr. 2018;58(2):262-296. (PubMed)
53. Schwingshackl L, Missbach B, Konig J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr. 2015;18(7):1292-1299. (PubMed)
54. Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA. 2015;313(19):1973-1974. (PubMed)
55. Chen JP, Chen GC, Wang XP, Qin L, Bai Y. Dietary fiber and metabolic syndrome: a meta-analysis and review of related mechanisms. Nutrients. 2017;10(1). (PubMed)
56. Wei B, Liu Y, Lin X, Fang Y, Cui J, Wan J. Dietary fiber intake and risk of metabolic syndrome: A meta-analysis of observational studies. Clin Nutr. 2018;37(6 Pt A):1935-1942. (PubMed)
57. Bradbury KE, Appleby PN, Key TJ. Fruit, vegetable, and fiber intake in relation to cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Am J Clin Nutr. 2014;100 Suppl 1:394s-398s. (PubMed)
58. Ben Q, Sun Y, Chai R, Qian A, Xu B, Yuan Y. Dietary fiber intake reduces risk for colorectal adenoma: a meta-analysis. Gastroenterology. 2014;146(3):689-699.e686. (PubMed)
59. Gianfredi V, Salvatori T, Villarini M, Moretti M, Nucci D, Realdon S. Is dietary fibre truly protective against colon cancer? A systematic review and meta-analysis. Int J Food Sci Nutr. 2018;69(8):904-915. (PubMed)
60. Ma Y, Hu M, Zhou L, et al. Dietary fiber intake and risks of proximal and distal colon cancers: A meta-analysis. Medicine (Baltimore). 2018;97(36):e11678. (PubMed)
61. McRae MP. The benefits of dietary fiber intake on reducing the risk of cancer: an umbrella review of meta-analyses. J Chiropr Med. 2018;17(2):90-96. (PubMed)
62. Bultman SJ. Molecular pathways: gene-environment interactions regulating dietary fiber induction of proliferation and apoptosis via butyrate for cancer prevention. Clin Cancer Res. 2014;20(4):799-803. (PubMed)
63. Kosumi K, Mima K, Baba H, Ogino S. Dysbiosis of the gut microbiota and colorectal cancer: the key target of molecular pathological epidemiology. J Lab Precis Med. 2018;3. (PubMed)
64. Ubeda C, Djukovic A, Isaac S. Roles of the intestinal microbiota in pathogen protection. Clin Transl Immunology. 2017;6(2):e128. (PubMed)
65. Encarnacao JC, Abrantes AM, Pires AS, Botelho MF. Revisit dietary fiber on colorectal cancer: butyrate and its role on prevention and treatment. Cancer Metastasis Rev. 2015;34(3):465-478. (PubMed)
66. Sivaprakasam S, Prasad PD, Singh N. Benefits of short-chain fatty acids and their receptors in inflammation and carcinogenesis. Pharmacol Ther. 2016;164:144-151. (PubMed)
67. Alberts DS, Martinez ME, Roe DJ, et al. Lack of effect of a high-fiber cereal supplement on the recurrence of colorectal adenomas. Phoenix Colon Cancer Prevention Physicians' Network. N Engl J Med. 2000;342(16):1156-1162. (PubMed)
68. DeCosse JJ, Miller HH, Lesser ML. Effect of wheat fiber and vitamins C and E on rectal polyps in patients with familial adenomatous polyposis. J Natl Cancer Inst. 1989;81(17):1290-1297. (PubMed)
69. Ishikawa H, Akedo I, Otani T, et al. Randomized trial of dietary fiber and Lactobacillus casei administration for prevention of colorectal tumors. Int J Cancer. 2005;116(5):762-767. (PubMed)
70. MacLennan R, Macrae F, Bain C, et al. Randomized trial of intake of fat, fiber, and beta carotene to prevent colorectal adenomas. J Natl Cancer Inst. 1995;87(23):1760-1766. (PubMed)
71. McKeown-Eyssen GE, Bright-See E, Bruce WR, et al. A randomized trial of a low fat high fibre diet in the recurrence of colorectal polyps. Toronto Polyp Prevention Group. J Clin Epidemiol. 1994;47(5):525-536. (PubMed)
72. Bonithon-Kopp C, Kronborg O, Giacosa A, Rath U, Faivre J. Calcium and fibre supplementation in prevention of colorectal adenoma recurrence: a randomised intervention trial. European Cancer Prevention Organisation Study Group. Lancet. 2000;356(9238):1300-1306. (PubMed)
73. Schatzkin A, Lanza E, Corle D, et al. Lack of effect of a low-fat, high-fiber diet on the recurrence of colorectal adenomas. Polyp Prevention Trial Study Group. N Engl J Med. 2000;342(16):1149-1155. (PubMed)
74. Yao Y, Suo T, Andersson R, et al. Dietary fibre for the prevention of recurrent colorectal adenomas and carcinomas. Cochrane Database Syst Rev. 2017;1:Cd003430. (PubMed)
75. Aune D, Chan DS, Greenwood DC, et al. Dietary fiber and breast cancer risk: a systematic review and meta-analysis of prospective studies. Ann Oncol. 2012;23(6):1394-1402. (PubMed)
76. Chen S, Chen Y, Ma S, et al. Dietary fibre intake and risk of breast cancer: A systematic review and meta-analysis of epidemiological studies. Oncotarget. 2016;7(49):80980-80989. (PubMed)
77. National Cancer Institute. Cancer causes and prevention: hormones. Available at: https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones. Accessed 3/1/19.
78. Rock CL, Flatt SW, Thomson CA, et al. Effects of a high-fiber, low-fat diet intervention on serum concentrations of reproductive steroid hormones in women with a history of breast cancer. J Clin Oncol. 2004;22(12):2379-2387. (PubMed)
79. Kasim-Karakas SE, Almario RU, Gregory L, Todd H, Wong R, Lasley BL. Effects of prune consumption on the ratio of 2-hydroxyestrone to 16alpha-hydroxyestrone. Am J Clin Nutr. 2002;76(6):1422-1427. (PubMed)
80. Manoj G, Thampi BS, Leelamma S, Menon PV. Effect of dietary fiber on the activity of intestinal and fecal beta-glucuronidase activity during 1,2-dimethylhydrazine induced colon carcinogenesis. Plant Foods Hum Nutr. 2001;56(1):13-21. (PubMed)
81. Fernandez MF, Reina-Perez I, Astorga JM, Rodriguez-Carrillo A, Plaza-Diaz J, Fontana L. Breast cancer and its relationship with the ,icrobiota. Int J Environ Res Public Health. 2018;15(8). (PubMed)
82. Landete JM. Plant and mammalian lignans: A review of source, intake, metabolism, intestinal bacteria and health. Food Research International. 2012;46(1):410-424.
83. Chen K, Zhao Q, Li X, et al. Dietary fiber intake and endometrial cancer risk: a systematic review and meta-analysis. Nutrients. 2018;10(7). (PubMed)
84. Coleman HG, Murray LJ, Hicks B, et al. Dietary fiber and the risk of precancerous lesions and cancer of the esophagus: a systematic review and meta-analysis. Nutr Rev. 2013;71(7):474-482. (PubMed)
85. Sun L, Zhang Z, Xu J, Xu G, Liu X. Dietary fiber intake reduces risk for Barrett's esophagus and esophageal cancer. Crit Rev Food Sci Nutr. 2017;57(13):2749-2757. (PubMed)
86. Zhang Z, Xu G, Ma M, Yang J, Liu X. Dietary fiber intake reduces risk for gastric cancer: a meta-analysis. Gastroenterology. 2013;145(1):113-120.e3. (PubMed)
87. Xu H, Ding Y, Xin X, Wang W, Zhang D. Dietary fiber intake is associated with a reduced risk of ovarian cancer: a dose-response meta-analysis. Nutr Res. 2018;57:1-11. (PubMed)
88. Huang X, Wang X, Shang J, et al. Association between dietary fiber intake and risk of ovarian cancer: a meta-analysis of observational studies. J Int Med Res. 2018;46(10):3995-4005. (PubMed)
89. Wang CH, Qiao C, Wang RC, Zhou WP. Dietary fiber intake and pancreatic cancer risk: a meta-analysis of epidemiologic studies. Sci Rep. 2015;5:10834. (PubMed)
90. Mao QQ, Lin YW, Chen H, et al. Dietary fiber intake is inversely associated with risk of pancreatic cancer: a meta-analysis. Asia Pac J Clin Nutr. 2017;26(1):89-96. (PubMed)
91. Sheng T, Shen RL, Shao H, Ma TH. No association between fiber intake and prostate cancer risk: a meta-analysis of epidemiological studies. World J Surg Oncol. 2015;13:264. (PubMed)
92. Wang RJ, Tang JE, Chen Y, Gao JG. Dietary fiber, whole grains, carbohydrate, glycemic index, and glycemic load in relation to risk of prostate cancer. Onco Targets Ther. 2015;8:2415-2426. (PubMed)
93. Huang TB, Ding PP, Chen JF, et al. Dietary fiber intake and risk of renal cell carcinoma: evidence from a meta-analysis. Med Oncol. 2014;31(8):125. (PubMed)
94. Singh V, Yeoh BS, Chassaing B, et al. Dysregulated microbial fermentation of soluble fiber induces cholestatic liver cancer. Cell. 2018;175(3):679-694.e622. (PubMed)
95. Kamarul Zaman M, Chin KF, Rai V, Majid HA. Fiber and prebiotic supplementation in enteral nutrition: A systematic review and meta-analysis. World J Gastroenterol. 2015;21(17):5372-5381. (PubMed)
96. Staller K, Song M, Grodstein F, et al. Increased long-term dietary fiber intake is associated with a decreased risk of fecal incontinence in older women. Gastroenterology. 2018;155(3):661-667.e661. (PubMed)
97. Bliss DZ, Savik K, Jung HJ, Whitebird R, Lowry A, Sheng X. Dietary fiber supplementation for fecal incontinence: a randomized clinical trial. Res Nurs Health. 2014;37(5):367-378. (PubMed)
98. Markland AD, Burgio KL, Whitehead WE, et al. Loperamide versus psyllium fiber for treatment of fecal incontinence: the fecal incontinence prescription (Rx) management (FIRM) randomized clinical trial. Dis Colon Rectum. 2015;58(10):983-993. (PubMed)
99. Hervik AK, Svihus B. The role of fiber in energy balance. J Nutr Metab. 2019;2019:4983657. (PubMed)
100. Clark MJ, Slavin JL. The effect of fiber on satiety and food intake: a systematic review. J Am Coll Nutr. 2013;32(3):200-211. (PubMed)
101. Wanders AJ, van den Borne JJ, de Graaf C, et al. Effects of dietary fibre on subjective appetite, energy intake and body weight: a systematic review of randomized controlled trials. Obes Rev. 2011;12(9):724-739. (PubMed)
102. Jane M, McKay J, Pal S. Effects of daily consumption of psyllium, oat bran and polyGlycopleX on obesity-related disease risk factors: A critical review. Nutrition. 2019;57:84-91. (PubMed)
103. Pal S, Ho S, Gahler RJ, Wood S. Effect on body weight and composition in overweight/obese Australian adults over 12 months consumption of two different types of fibre supplementation in a randomized trial. Nutr Metab (Lond). 2016;13:82. (PubMed)
104. Huang T, Xu M, Lee A, Cho S, Qi L. Consumption of whole grains and cereal fiber and total and cause-specific mortality: prospective analysis of 367,442 individuals. BMC Med. 2015;13:59. (PubMed)
105. Chan CW, Lee PH. Association between dietary fibre intake with cancer and all-cause mortality among 15 740 adults: the National Health and Nutrition Examination Survey III. J Hum Nutr Diet. 2016;29(5):633-642. (PubMed)
106. Liu L, Wang S, Liu J. Fiber consumption and all-cause, cardiovascular, and cancer mortalities: a systematic review and meta-analysis of cohort studies. Mol Nutr Food Res. 2015;59(1):139-146. (PubMed)
107. Hajishafiee M, Saneei P, Benisi-Kohansal S, Esmaillzadeh A. Cereal fibre intake and risk of mortality from all causes, CVD, cancer and inflammatory diseases: a systematic review and meta-analysis of prospective cohort studies. Br J Nutr. 2016;116(2):343-352. (PubMed)
108. Anderson JW, Randles KM, Kendall CW, Jenkins DJ. Carbohydrate and fiber recommendations for individuals with diabetes: a quantitative assessment and meta-analysis of the evidence. J Am Coll Nutr. 2004;23(1):5-17. (PubMed)
109. MacLeod J, Franz MJ, Handu D, et al. Academy of Nutrition and Dietetics Nutrition practice guideline for type 1 and type 2 diabetes in adults: nutrition intervention evidence reviews and recommendations. J Acad Nutr Diet. 2017;117(10):1637-1658. (PubMed)
110. Dietary Guidelines Advisory Committee. 2015. Scientific Report of the 2015 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. U.S. Department of Agriculture, Agricultural Research Service, Washington, D.C. Available at: https://health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf. Accessed 3/18/19.
111. Huo R, Du T, Xu Y, et al. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur J Clin Nutr. 2015;69(11):1200-1208. (PubMed)
112. Jovanovski E, Khayyat R, Zurbau A, et al. Should viscous fiber supplements be considered in diabetes control? Results from a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2019;42(5):755-766. (PubMed)
113. McRorie JWJ, Gibb RD, Womack JB, Pambianco DJ. Psyllium is superior to wheat dextrin for lowering elevated serum cholesterol. Nutrition Today. 2017;52(6):289-294. Available at: https://journals.lww.com/nutritiontodayonline/Fulltext/2017/11000/Psyllium_Is_Superior_to_Wheat_Dextrin_for_Lowering.8.aspx.
114. Jenkins DJ, Kendall CW, Augustin LS, et al. Effect of wheat bran on glycemic control and risk factors for cardiovascular disease in type 2 diabetes. Diabetes Care. 2002;25(9):1522-1528. (PubMed)
115. Prasad VG, Abraham P. Management of chronic constipation in patients with diabetes mellitus. Indian J Gastroenterol. 2017;36(1):11-22. (PubMed)
116. American College of Gastroenterology Chronic Constipation Task Force. An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol. 2005;100 Suppl 1:S1-4. (PubMed)
117. Dahl WJ, Mendoza DR. Is fibre an effective strategy to improve laxation in long-term care residents? Can J Diet Pract Res. 2018;79(1):35-41. (PubMed)
118. Rungsiprakarn P, Laopaiboon M, Sangkomkamhang US, Lumbiganon P, Pratt JJ. Interventions for treating constipation in pregnancy. Cochrane Database Syst Rev. 2015(9):Cd011448. (PubMed)
119. Turawa EB, Musekiwa A, Rohwer AC. Interventions for treating postpartum constipation. Cochrane Database Syst Rev. 2014(9):Cd010273. (PubMed)
120. Bharucha AE, Pemberton JH, Locke GR, 3rd. American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144(1):218-238. (PubMed)
121. Ford AC, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol. 2014;109 Suppl 1:S2-26; quiz S27. (PubMed)
122. Defrees DN, Bailey J. Irritable bowel syndrome: epidemiology, pathophysiology, diagnosis, and treatment. Prim Care. 2017;44(4):655-671. (PubMed)
123. Varju P, Farkas N, Hegyi P, et al. Low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet improves symptoms in adults suffering from irritable bowel syndrome (IBS) compared to standard IBS diet: A meta-analysis of clinical studies. PLoS One. 2017;12(8):e0182942. (PubMed)
124. Moayyedi P, Quigley EM, Lacy BE, et al. The effect of fiber supplementation on irritable bowel syndrome: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109(9):1367-1374. (PubMed)
125. Nagarajan N, Morden A, Bischof D, et al. The role of fiber supplementation in the treatment of irritable bowel syndrome: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2015;27(9):1002-1010. (PubMed)
126. Rezapour M, Ali S, Stollman N. Diverticular disease: an update on pathogenesis and management. Gut Liver. 2018;12(2):125-132. (PubMed)
127. Korzenik JR. Case closed? Diverticulitis: epidemiology and fiber. J Clin Gastroenterol. 2006;40 Suppl 3:S112-116. (PubMed)
128. Painter NS, Burkitt DP. Diverticular disease of the colon: a deficiency disease of Western civilization. Br Med J. 1971;2(5759):450-454. (PubMed)
129. Peery AF, Barrett PR, Park D, et al. A high-fiber diet does not protect against asymptomatic diverticulosis. Gastroenterology. 2012;142(2):266-72.e1. (PubMed)
130. Carabotti M, Annibale B, Severi C, Lahner E. Role of fiber in symptomatic uncomplicated diverticular disease: a systematic review. Nutrients. 2017;9(2). (PubMed)
131. Dahl C, Crichton M, Jenkins J, et al. Evidence for dietary fibre modification in the recovery and prevention of reoccurrence of acute, uncomplicated diverticulitis: a systematic literature review. Nutrients. 2018;10(2). (PubMed)
132. Floch MH, Longo WE. United States guidelines for diverticulitis treatment. J Clin Gastroenterol. 2016;50 Suppl 1:S53-56. (PubMed)
133. Galetin T, Galetin A, Vestweber KH, Rink AD. Systematic review and comparison of national and international guidelines on diverticular disease. Int J Colorectal Dis. 2018;33(3):261-272. (PubMed)
134. Webster DJ, Gough DC, Craven JL. The use of bulk evacuant in patients with haemorrhoids. Br J Surg. 1978;65(4):291-292. (PubMed)
135. Perez-Miranda M, Gomez-Cedenilla A, Leon-Colombo T, Pajares J, Mate-Jimenez J. Effect of fiber supplements on internal bleeding hemorrhoids. Hepatogastroenterology. 1996;43(12):1504-1507. (PubMed)
136. Garg P, Singh P. Adequate dietary fiber supplement and TONE can help avoid surgery in most patients with advanced hemorrhoids. Minerva Gastroenterol Dietol. 2017;63(2):92-96. (PubMed)
137. Reicks M, Jonnalagadda S, Albertson AM, Joshi N. Total dietary fiber intakes in the US population are related to whole grain consumption: results from the National Health and Nutrition Examination Survey 2009 to 2010. Nutr Res. 2014;34(3):226-234. (PubMed)
138. Marlett JA. Content and composition of dietary fiber in 117 frequently consumed foods. J Am Diet Assoc. 1992;92(2):175-186. (PubMed)
139. Food and Drug Administration. Import Alert 33-15: detention without physical examination of gel candies containing konjac. Available at: https://www.accessdata.fda.gov/cms_ia/importalert_105.html. Accessed 7/11/19.
140. Gibson GR, Beatty ER, Wang X, Cummings JH. Selective stimulation of bifidobacteria in the human colon by oligofructose and inulin. Gastroenterology. 1995;108(4):975-982. (PubMed)
141. Kolida S, Tuohy K, Gibson GR. Prebiotic effects of inulin and oligofructose. Br J Nutr. 2002;87 Suppl 2:S193-197. (PubMed)
142. Cummings JH, Macfarlane GT. Gastrointestinal effects of prebiotics. Br J Nutr. 2002;87 Suppl 2:S145-151. (PubMed)
143. Pittler MH, Ernst E. Guar gum for body weight reduction: meta-analysis of randomized trials. Am J Med. 2001;110(9):724-730. (PubMed)
144. Huang H, Zou Y, Chi H, Liao D. Lipid-modifying effects of chitosan supplementation in humans: a pooled analysis with trial sequential analysis. Mol Nutr Food Res. 2018;62(8):e1700842. (PubMed)
145. Moraru C, Mincea MM, Frandes M, Timar B, Ostafe V. A meta-analysis on randomised controlled clinical trials evaluating the effect of the dietary supplement chitosan on weight loss, lipid parameters and blood pressure. Medicina (Kaunas). 2018;54(6). (PubMed)
146. American Academy of Family Physicians. Fiber: how to increase the amount in your diet [Web page]. August 2020. Available at: https://familydoctor.org/fiber-how-to-increase-the-amount-in-your-diet/. Accessed 1/3/22.
147. Papazian R. Bulking up fiber's healthful reputation. Food and Drug Administration, [Web page]. October 26, 1998. http://www.fda.gov/fdac/features/1997/597_fiber.html. Accessed 9/14/04.
148. Rosario PG, Gerst PH, Prakash K, Albu E. Dentureless distention: oat bran bezoars cause obstruction. J Am Geriatr Soc. 1990;38(5):608. (PubMed)
149. Miller DL, Miller PF, Dekker JJ. Small-bowel obstruction from bran cereal. JAMA. 1990;263(6):813-814. (PubMed)
150. Cooper SG, Tracey EJ. Small-bowel obstruction caused by oat-bran bezoar. N Engl J Med. 1989;320(17):1148-1149. (PubMed)
151. McClurken JB, Carp NZ. Bran-induced small-intestinal obstruction in a patient with no history of abdominal operation. Arch Surg. 1988;123(1):98-100. (PubMed)
152. McRorie Jr JW, Fahey Jr GC. Fiber supplements and clinically meaningful health benefits: Identifying the physiochemical characteristics of fiber that drive specific physiologic effects. Dietary Supplements in Health Promotion: CRC Press; 2015:172-217.
153. Lewis JH. Esophageal and small bowel obstruction from guar gum-containing "diet pills": analysis of 26 cases reported to the Food and Drug Administration. Am J Gastroenterol. 1992;87(10):1424-1428. (PubMed)
154. Agha FP, Nostrant TT, Fiddian-Green RG. "Giant colonic bezoar:" a medication bezoar due to psyllium seed husks. Am J Gastroenterol. 1984;79(4):319-321. (PubMed)
155. Schneider RP. Perdiem causes esophageal impaction and bezoars. South Med J. 1989;82(11):1449-1450. (PubMed)
156. Chandra R, Barron JL. Anaphylactic reaction to intravenous sinistrin (Inutest). Ann Clin Biochem. 2002;39(Pt 1):76. (PubMed)
157. Gay-Crosier F, Schreiber G, Hauser C. Anaphylaxis from inulin in vegetables and processed food. N Engl J Med. 2000;342(18):1372. (PubMed)
158. Khalili B, Bardana EJ, Jr., Yunginger JW. Psyllium-associated anaphylaxis and death: a case report and review of the literature. Ann Allergy Asthma Immunol. 2003;91(6):579-584. (PubMed)
159. Fugh-Berman A. Herb-drug interactions. Lancet. 2000;355(9198):134-138. (PubMed)
160. Richter WO, Jacob BG, Schwandt P. Interaction between fibre and lovastatin. Lancet. 1991;338(8768):706. (PubMed)
161. Greger JL. Nondigestible carbohydrates and mineral bioavailability. J Nutr. 1999;129(7 Suppl):1434S-1435S. (PubMed)
162. Bosscher D, Van Caillie-Bertrand M, Van Cauwenbergh R, Deelstra H. Availabilities of calcium, iron, and zinc from dairy infant formulas is affected by soluble dietary fibers and modified starch fractions. Nutrition. 2003;19(7-8):641-645. (PubMed)
163. Scholz-Ahrens KE, Schrezenmeir J. Inulin, oligofructose and mineral metabolism - experimental data and mechanism. Br J Nutr. 2002;87 Suppl 2:S179-186. (PubMed)
164. Rock CL, Swendseid ME. Plasma beta-carotene response in humans after meals supplemented with dietary pectin. Am J Clin Nutr. 1992;55(1):96-99. (PubMed)
165. Riedl J, Linseisen J, Hoffmann J, Wolfram G. Some dietary fibers reduce the absorption of carotenoids in women. J Nutr. 1999;129(12):2170-2176. (PubMed)